 In a recent analysis of 150 patients with post-thrombotic syndrome included in the Swiss and Arnsberg venous stent registries, braided as compared with laser-cut nitinol stents for common femoral vein obstruction appeared to be associated with favourable primary patency at 12 months.
In a recent analysis of 150 patients with post-thrombotic syndrome included in the Swiss and Arnsberg venous stent registries, braided as compared with laser-cut nitinol stents for common femoral vein obstruction appeared to be associated with favourable primary patency at 12 months.
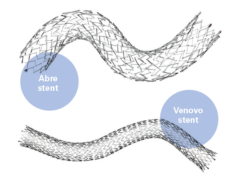
The authors—Laura Moeri (University Hospital Zurich, Zurich, Switzerland) and colleagues—detail that braided nitinol stents may be less prone to fractures and reocclusion at the inguinal ligament.
Writing the Journal of Vascular Surgery: Venous and Lymphatic Disorders, Moeri and colleagues note that chronic obstruction of the common femoral vein in patients with post-thrombotic syndrome after iliofemoral or iliocaval deep vein thrombosis remains a challenge for endovascular treatment. They add that patency rates and clinical outcomes of laser-cut and braided nitinol stents extending to the common femoral vein have not been studied yet.
From the Swiss and Arnsberg venous stent registries, the investigators included 150 post-thrombotic syndrome patients (mean age 44±16 years, 48% women) with laser-cut (n=101) and braided nitinol (n=49) stents placed into the common femoral vein across the inguinal ligament. Routine follow-up included duplex ultrasound examinations and assessment of clinical scores, and the primary study outcome was primary and secondary patency at 12 months.
Overall, the mean number of implanted stents was 2.6±1.7. The proximal stent landing zone was the inferior vena cava in 32 (21%) patients, the iliac vein in 106 (76%), and the common femoral vein in 5 (3%).
Moeri and colleagues report that the primary patency rate was 67.3% (95% confidence interval [CI] 58–76.6%) in the laser-cut and 86.7% (95% CI 75–98.1%) in the braided stent group (logrank p=0.016). Secondary patency rate was 93.9% (95% CI 89.2–98.6) and 100% respectively (logrank p=0.1).
The median improvement in Villalta score from baseline to the latest follow-up was 4 (interquartile range [IQR]: 2–6) points, without difference between the groups.
Symptomatic common femoral vein stent fractures were observed in four (4%) patients with laser-cut stents and in no patient with a braided stent.
In the discussion of their findings, Moeri et al acknowledge several limitations of the study. One drawback was the shorter follow-up time in the braided nitinol group was shorter; “patency rates and clinical outcomes may become clearer with longer follow-up,” they write. In addition, although baseline characteristics of the two groups appeared comparable, the study was not randomised and therefore the patency rates in the two stent groups cannot be directly compared.
The authors conclude that a substantial proportion of post-thrombotic syndrome patients with stents in the common femoral vein may experience stent occlusion, which appeared to be particularly the case in patients treated with a laser-cut stent. “In some cases,” the authors note, “stent fracturing was suspected to be the cause of loss of patency”. Nevertheless, they observed an overall improvement in clinical post-thrombotic syndrome scores and high rates of secondary patency.
Looking ahead, Moeri and colleagues write that long-term studies are needed to confirm that braided nitinol stents in the common femoral vein may be less prone to fractures.