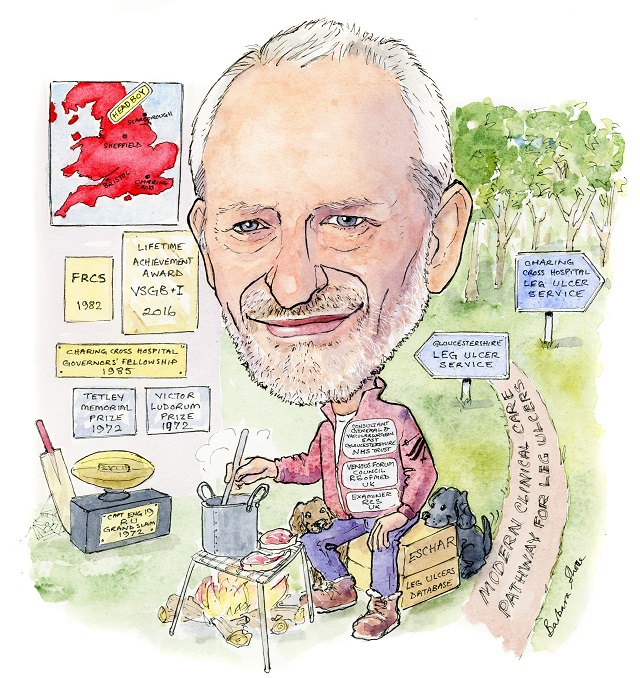
 Coming from a non-medical background, Keith Poskitt is unable to pinpoint exactly how his interest in the field developed. At school, science, and sports—rugby and cricket in particular—vied for his attention. Following a serious ankle injury at the age of 19, any dreams of a sporting career were dashed. Luckily for the venous field, this set Poskitt firmly on the medicinal career path. He spoke to Venous News about the current state of venous medicine, what future developments he is keeping tabs on, and the important personal and professional lessons he has learned over the course of his varied and influential career.
Coming from a non-medical background, Keith Poskitt is unable to pinpoint exactly how his interest in the field developed. At school, science, and sports—rugby and cricket in particular—vied for his attention. Following a serious ankle injury at the age of 19, any dreams of a sporting career were dashed. Luckily for the venous field, this set Poskitt firmly on the medicinal career path. He spoke to Venous News about the current state of venous medicine, what future developments he is keeping tabs on, and the important personal and professional lessons he has learned over the course of his varied and influential career.
Why did you decide you wanted a career in medicine, and why in particular did you choose to enter the vascular and venous fields?
As I came from a non-medical family, I am unsure exactly where my interest in medicine developed, but it is quite clear to me now that it was the correct choice of profession. My career has been demanding but thoroughly enjoyable, dare I say fun! The attraction to a medical career developed in my early teenage years at a time when I found science subjects more stimulating than the alternatives with the exception of the sports periods. My interest in vascular surgery developed while working as a surgical houseman for Chris Rigby who was an inspiring general/vascular surgeon in Rotherham—he made work rewarding and enjoyable! Who have been your most important career mentors and what wisdom did they impart? Moving south from Yorkshire to work in the “big city” at Charing Cross Hospital with Professor Roger Greenhalgh and then Charles McCollum was a major step in my surgical career. Charing Cross was hugely influential in many ways, not only clinically, but academically and socially. My obsessional nature allowed me to learn in this highly organised, forward-thinking environment where I was exposed to high-quality research, multidisciplinary team meetings, teamwork, and non-invasive vascular assessment. Within a short time of arriving in London, the young Yorkshireman was invited to dinner with Princess Anne (and about 200 others) at Hampton Court Palace as a delegate at the 1982 Charing Cross Symposium. This was different! I gained invaluable experience when mentored in Bristol working with both Roger Baird and Mike Horrocks. The philosophical mind of Roger Baird was inspirational and Mike Horrocks’ drive for perfection was infectious. In addition to gaining major experience in carotid and open aortic surgery, I was introduced to endoscopic surgery and helped facilitate the introduction of a new minimally invasive technique of transthoracic endoscopic sympathectomy for hyperhidrosis. A major learning point that I have taken forward with me in my career is the invaluable art of departmental surgical audit which offers an important tool to use in order to reflect, study outcomes and report results.
What has been the biggest development in venous medicine during the course of your career?
The introduction of duplex scanning has revolutionised both arterial and venous investigation and endovenous treatments for venous reflux have had a major effect on the management of venous dysfunction. What is the most interesting paper or presentation that you have seen recently (aside from your own research)? I am fascinated by stem cell publications. Although the minimally invasive world of laparoscopic surgery and endovascular interventions have revolutionised surgical treatments, I believe the major developments over the next 10–15 years will be in the developing areas of biological engineering and stem cell research. These areas have enormous potential for modifying surgical practice with ongoing research addressing both the engineering and biomedical hurdles with the potential of delivering cellular building blocks to deal with occlusive arterial disease and venous ulceration.
What are your current research interests?
Following the ESCHAR study, our unit has collaborated with other venous experts including Alun Davies, Andrew Bradbury, Isaac Nyamekye and Manj Gohel to form a strong collaborative venous research group. The Cheltenham unit has become the lead recruiting centre for the EVRA (Early Venous Reflux Ablation) leg ulcer study. The results of this large randomised controlled trial will be available later in the year and will provide further high-quality information on managing chronic venous ulceration. You were involved in the 2013 NICE UK guidelines on varicose vein treatment – how have these guidelines affected your practice? Sadly the NHS is a postcode lottery and as yet the local commissioners have failed to accept that they should fund endothermal venous treatment! Is there still a place for open surgery in varicose vein treatment? Never say never. Only very rarely for those refluxing trunks with a very large diameter.
Data from the ATTRACT trial has recently been announced, failing to meet its primary endpoints—what impact do you think that this will have on venous practice?
Research always poses more questions than answers and demonstrating a treatment option is no better than an alternative is still of great value. In this study, it is possible that the methods of lysis and stents used were not ideal and could be improved. One other comment is that the study design had entry criteria that were possibly too broad—a more focussed population aiming at specific target vessels may be more appropriate, ie. should the study have initially assessed occluded veins proximal to the profunda vein?
One of your areas of interest is venous ulcers—what latest research and/or treatments are you keeping an eye on in this area?
In my view, the most important area of research in chronic venous leg ulceration is the modification of the underlying abnormal pathophysiology. With the introduction of venous duplex and endovenous ablation techniques, superficial venous reflux management has improved ulceration outcomes. The non-invasive detection of chronic venous ulceration resulting from underlying proximal iliac vein stenosis/occlusion needs continued development when present in isolation and presenting in combination with superficial venous reflux.
How important is it to look at the prevention of venous ulcers as well as treating them when they occur? What advances and concepts currently interest you in this area?
Both are important. It is of paramount importance to understand the mechanism of the treatments of compression and superficial venous ablation in isolation and when used in combination. In patients with venous leg ulceration resulting from superficial venous reflux, compression alone or superficial venous ablation alone will facilitate ulcer healing. In my view, when compression is poorly tolerated or suboptimal compression is applied, early superficial ablation is likely to speed up healing. If high-quality compression is applied, it is unlikely that additional early superficial venous ablation will confer any additional benefits with regard to healing. As persistent capillary hypertension is the primary cause of chronic venous ulceration, an area of interest is Bush’s concept of TIRS (Terminal interruption of refluxing source), particularly in those limbs with total deep venous reflux.
Could you tell us about one of your most memorable cases? What did this experience teach you?
A few years ago, I was reminded of a case I performed when I was a senior registrar when life was different. I had been asked to hold the fort for transplant on call when one consultant was recovering from surgery and another consultant mentor, Barry Pentlow, was having a deserved holiday break. A donor’s kidney became available for a brave five-year-old boy who had had two earlier transplant rejections. Both iliac systems had been used previously so surgical options were limited. With no other option at the time and some degree of apprehension, I carried out the renal transplant using the aorta and vena cava for inflow and outflow respectively and was delighted that the surgery was uneventful. More rewarding however was the subsequent feedback some 20-odd years later when I was informed by Barry Pentlow at a vascular conference that the young five-year-old was a thriving adult approaching 30. I am not sure that you always learn from all cases but feedback is rewarding to all and reminds you why you love the job you do. The second case I remember well was a lorry driver who was admitted with abdominal and back pain. He had parked up his truck in a service station off the motorway and had tried to sleep overnight in his truck but eventually rang his wife 150 miles away who thought it best to ring for an ambulance. He was seen in accident and emergency and diagnosed with a ruptured abdominal aortic aneurysm and taken to theatre immediately. Having been called, I arrived in the theatre to see our patient on the operating table, surrounded by anesthetists and nurses with a flurry of activity. I quickly assessed his abdomen and explained the problem and what we planned to do. I was on my way to scrub up when he called me back. The room fell silent and with a serious look on his face, he informed me that if anything untoward happened which required him having mouth-to-mouth resuscitation, he would prefer one of the nurses giving it rather than me! He concluded with a smile and I just knew all would turn out well. The final case I wish to share with you is a patient who has become a great friend to both me and the department. Our paths first crossed 15 years ago when he had a small stroke associated with tight stenosis of his internal carotid artery. In order to demonstrate the eversion carotid endarterectomy technique at the Vascular Society, I obtained his consent to video the procedure and on every subsequent occasion I saw him, he teased me about still owing him the “fee” for the filming. Some years passed before we met up in different circumstances when he came to see me suffering from a painful circumferential leg ulcer of two years’ duration. Following a venous duplex, we treated his leg with compression, duplex guided foam sclerotherapy and pinch skin grafting under local anesthetic. While carrying out the skin grafting, there was the reassuring but annoying beeping from the heart monitor and when he asked what would happen if the beeping stopped, I paused for thought and, knowing him well, simply said: “We would all probably go home a little earlier!” His leg ulcer healed and has not recurred.
What are some of the proudest moments in your career?
- 1972: Winning the Grand Slam as captain of the England 19 group in Rugby Union.
- 1982: Being presented with my Fellowship at the Royal College of Surgeons (in front of my mum).
- 2006: Following mentorship from both Ralf Kolvenbach and Marc Coggia, my colleague Mark Whyman and I performed the first total laparoscopic abdominal aortic aneurysm repair in the UK. We have now performed over a hundred laparoscopic cases with a mortality of 2%.
- 2016: Recipient of Lifetime Achievement Award from the Vascular Society of Great Britain and Ireland.
What three questions in venous medicine still need to be answered?
- Would chronic venous ulcer management improve by introducing a structured National Leg Ulcer Service?
- Is it feasible to prevent the development of the post-thrombotic limb following major proximal venous thrombosis?
- Could complications of venous hypertension be reliably treated by improved deep venous valvular treatments?
What advice would you give to young surgeons starting out in their careers?
Do not expect anything to come easily in life. I have two favourite sporting quotes which also apply to surgery:
- Gary Player: “The harder you work the luckier you are”.
- Alex Ferguson: “Failure to prepare, prepare to fail”.
As a surgeon, you need both ability and experience and indeed ensure that you know how to deal with the simple things first before embarking on the more complex. Sharing ideas and working with a colleague or within a team is beneficial to patients and enjoyable for the team. Surgery, in particular, vascular surgery, is very different compared to 30 years ago. Young surgeons should continue to expect and embrace change.
What are some of your hobbies and interests outside of medicine?
Sport played the leading role in my life in my early years playing rugby and cricket to a serious level. However, at 19, a badly fractured ankle upset my dreams and changed my focus from rugby to medicine. A lesson to be learned— life can be cruel but may open up other opportunities. I treasure my trips to our apartment in the French Alps for skiing, walking, and food. My guilty pleasure is fire! I love nothing more than having a bonfire in our orchard usually trying to cook a “special dish” or enjoying a log fire on a rainy day watching an old movie after taking the wife and dogs for a walk. Is there anything else that you would like to mention that we have not yet covered? When asked to contribute this article to Venous News, my immediate thought was “thank you for asking but no thank you—it’s not me”. However, as you get older you may get wiser and after discussing the request with my wife (who is younger and wiser), she encouraged me to jot down a few lines and consider the request as an honour and by way of a thank you for my contribution to the patients over the years. I have been fortunate to have a career that I have enjoyed for 40 years and still look forward to reporting to work each morning!
Fact File
Education
1965–1972 Scarborough High School for Boys, Yorkshire, UK
1972–1977 University of Sheffield Medical School, UK Current position
1989–present Consultant Surgeon, Gloucestershire Hospitals NHS Foundation Trust, UK
Previous appointments
1977–78 House Surgeon Rotherham, UK
1978 House Physician LMH, Sheffield, UK
1978–79 Surgical SHO NGH, Sheffield, UK
1979–80 Rotating Surgical SHO NGH, Sheffield, UK
1980–82 Rotating Surgical Registrar Hallamshire Hospital, Sheffield, UK
1982–85 Post Fellowship Registrar Professorial Unit, Charing Cross Hospital, London, UK
1983–84 Surgical Research Fellow Professorial Unit, Charing Cross Hospital, London, UK
1985–89 Senior Surgical Registrar South West Surgical Rotation, Southmead and BRI, Bristol, UK
Positions held
1992–98 Royal College of Surgeons Surgical Tutor, UK
1998–2002 Programme Director of Surgery, South West Deanery, UK
2002–present Venous Forum Council, Royal Society of Medicine, UK
2002–present Examiner, Royal College of Surgeons, UK
2012–14 Guideline Development Group varicose veins, NICE Fact File












