
By Johann Chris Ragg
All stages of vein disease start from small and local disorders, and most of them manifest with increased vein diameters. The idea of restoring orthograde flow by normalising valve zone diameters has been followed for more than 10 years when performing “extraluminal valvuloplasty” by surgical grafting. This modality using PTFE, Dacron or polyurethane patches to surround and fix the valve zone gives proof of the principle. How-ever, surgery is too invasive to serve as an early stage method. Thermal shrinking via catheter approach has failed so far (remember “VNUS Restore”). Based on the experience of a modified “coaxial” perivenous tumescent anaesthesia (CPTA) used in more than 25,000 thermal endovenous procedures, valve zone shaping by perivenous injection of hyaluronan gels instead of fluids was attempted (Figure 1).
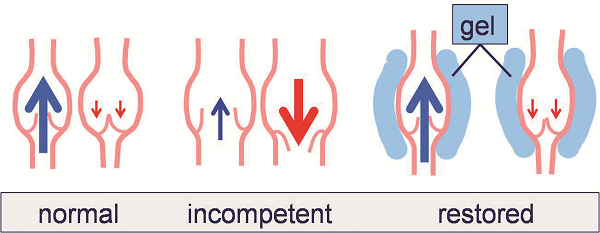
In a pilot study in 2014, 20 patients (12 females, 38–67 years old) with proximal valve incompetence of the great saphenous vein (diameter 7–11.4mm, mean 8.6) providing preserved and mobile valve structures were selected to receive a diameter reduction of the diseased valve zone by circumferential injection of a NASHA gel, 2% solution, crosslink degree 0.5–1%. Gel injections were performed by use of a novel safety system consisting of a relocatable cannula with triple-cut tip, and a flexible outer metal catheter (IntraShape, Venartis). The sharp tip is used to perforate skin and fasciae, and the blunt tip to move next to the vein, avoiding incidental vein puncture, and attempting circumferential distribution of the hyaluronan. All steps were performed under continuous ultrasound imaging. The injection was concluded when reflux was no longer observed in the standing patient (tilting table). No external compression was applied. Clinical and ultrasound examinations including video recordings were per-formed after two, 12, 26 and 52 weeks. An orthograde flow could be established in 19/20 cases (95%) using gel volumina of 14–35ml (mean: 21.3ml) (Figure 2).
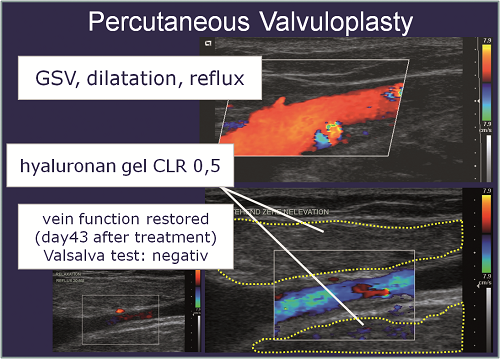
The treated segment length was 4–8cm (mean 5.1cm). After 12 weeks orthograde flow was present in 18/19 cases (83.3%), after 26 weeks in 15/19 cases (78.95%) and after 52 weeks in 13/19 cases (68.4%). All cases with remaining or recurring reflux (n=6) received a second gel injection of 4–7ml with haemodynamic success up to week 52 or beyond. There was no adverse reaction and no local discomfort. In a more recent and ongoing study another hyaluronan gel with optimised crosslinked NASHA microparticles of <0.2mm was used to allow more precise injections. Successful restoration of great saphenous vein valves could be established in 12/12 consecutive cases with gel volumes of just 3–8ml. In conclusion, percutaneous valvuloplasty is a feasible, effective and safe modality to restore proximal great saphenous vein valves in case of moderate dilatation and preserved valve structures. The procedure is minimally invasive and appropriate for preventive and early stage therapy. After a learning curve in placement technique and studies on substance longevity, first data may be expected to indicate if years of restoration can be accomplished without retreatment. Indications may be extended to later stages, combining with other endovenous modalities, and to further locations even including the deep venous system.
Johann Chris Ragg is founder and head of Angioclinic Vein Centers, Berlin, Munich, Germany, and Zurich, Switzerland. Work group website www.venartis.org












