At the Leipzig Interventional Course (LINC) 2024 (May 28–31, Leipzig, Germany), Michael Lichtenberg (Arnsberg Vascular Clinic, Arnsberg, Germany) shared for the first time a 24-month update from the P-MAX study of the Aspirex (BD) endovascular thrombectomy system in the treatment of acute venous occlusions. The study’s principal investigator highlighted procedural and technical success rates of 97.5% and a 24-month primary patency rate of 77.9% among other key findings.
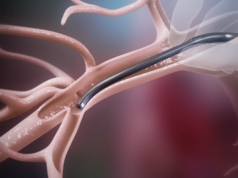
P-MAX is a prospective, multicentre, postmarket observational investigation designed to evaluate the outcomes of Aspirex in patients with deep vein thrombosis (DVT) of the pelvis, legs, and the inferior vena cava (IVC).
The study has enrolled patients at nine centres across the European Union, with follow-up already conducted for post-index procedure (discharge) and at one, six and 12 months. At LINC 2024, Lichtenberg shared 24-month follow-up data and noted that 36-month follow-up is also planned.
The presenter noted that patients over the age of 18 with acute thrombotic or thromboembolic occlusion (defined as the onset of pain within 14 days) and who signed a written informed consent form were included in the study. Key exclusion criteria included unsuitability for thrombectomy and known, unhealed, pre-existing mechanical damage to the vessel wall caused by surgical procedures or interventional complications, among other factors.
Lichtenberg shared with the LINC audience that 81 patients were enrolled in the study, consented to treatment, and subsequently treated with Aspirex. The mean age of these patients, he added, was 49.3±17.4 years, with 50.6% and 49.4% of the patients being male and female, respectively.
Regarding follow-up, Lichtenberg detailed that 80 (98.8%) patients completed one-month follow-up, reducing to 78 (96.3%) at six months, 74 (91.4%) at 12 months, and 66 (81.5%) at 24 months.
Lichtenberg provided some details on the medical history of the patients enrolled in the trial, noting that 21/81 (25.9%) were smokers, 5/81 (6.2%) had diabetes mellitus, 29/81 (35.8%) had hypertension, 11/81 (13.6%) were on systemic contraceptives, and 3/81 (3.7%) were undergoing cortisone therapy.
The presenter also detailed the key lesion characteristics of the 81 patients enrolled in the study. The mean target lesion length was 204.9mm, with a majority (70.4%) of the vessels occluded being veins, and the most common thrombus location being the external iliac vein (74.1%).
Procedural success in the P-MAX study was defined as intervention with Aspirex, with or without adjunctive treatment, being sufficient to remove the thrombus; maintain restored blood flow at least 72 hours post-intervention; avoid critical injuries at access site, route of catheter and target site; and be absent of acute distal embolism respective of pulmonary embolism. This was achieved in 79/81 (97.5%) patients.
Technical success was defined as a successful thrombectomy, which was achieved in 79/81 (97.5%) patients.
Primary patency was defined as freedom from reintervention, which was achieved in 79/80 (98.8%) patients at discharge, 75/80 (93.8%) at one month, 70/79 (88.6%) at six months, 62/72 (82.7%) at 12 months, and 53/68 (77.9%) at 24 months.
Safety was defined as serious adverse events (SAE) rate, procedure-related adverse events (AE) rate, and serious adverse device events (SADE) rate at one, six, 12 and 24 months.
Lichtenberg relayed that the SAE rate results were 27/81 (33.3%), 34/81 (42%), 40/80 (50%), and 46/77 (59.7%) at one, six, 12 and 24 months, respectively. The corresponding figures for AE rate were 11/80 (13.8%), 11/79 (13.9%), 11/74 (14.9%), and 11/66 (16.7%) and for SADE rate were 2/80 (2.5%), 2/79 (2.5%), 2.74 (2.7%), and 2/64 (3.1%).
In terms of secondary endpoints, the presenter reported that Venous Clinical Severity Score (VCSS), Venous Disability Score (VDS) and Clinical-Etiology-Anatomic-Pathophysiologic Score (CEAP) all improved from baseline—an improvement that he shared was sustained out to 24-month follow-up.
Speaking to Venous News following his presentation at LINC 2024, Lichtenberg commented: “Based on the very positive data from this study as well as others for mechanical thrombectomy, I suggest we stop thrombolysis therapy. Mechanical thrombectomy for iliofemoral DVT is safe and effective.”