Researchers from Norway have found that additional treatment with catheter-directed thrombolysis (CDT), when compared to standard treatment of oral anticoagulation therapy and elastic compression stockings, reduces the risk of post-thrombotic syndrome (PTS) in patients who suffer from deep-vein thrombosis (DVT) in their lower limbs.
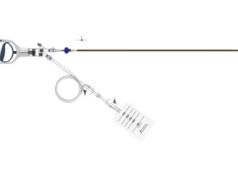
To reduce the risk of developing post-thrombotic syndrome, additional therapy is needed via catheter-directed thrombolysis, a minimally invasive procedure that uses x-ray imaging to administer medication to help dissolve clots through a catheter placed in the vein.
This procedure has become standard of care for the prevention of post-thrombotic syndrome in some treatment centres, despite a lack of randomised, controlled trials demonstrating its efficacy and safety, as well as several drawbacks including its high expense, association with life-threatening bleeding, and tendency to convert DVT (typically an outpatient condition) to an in-patient disease requiring hospitalisation.
To evaluate whether additional treatment of deep-vein thrombosis with CDT with alteplase reduces post-thrombotic syndrome development following acute iliofemoral DVT (occurring in the upper thigh and/or pelvic area), Enden et al embarked on the CAVENT (Catheter-directed venous thrombolysis in acute iliofemoral vein thrombosis) study, a large, four-year, multicentre, randomised controlled trial. The study was presented by Tone Ronnaug Enden, Oslo University Hospital, Norway, on 13 December at a late breaking trials session at the 53th American Society of Hematology meeting in San Diego, USA.
In this trial, 209 patients between the ages of 18 and 75 with a first-time acute iliofemoral DVT, with symptoms present for up to 21 days, were randomised into two treatment arms: Treatment arm A (the CDT-treated arm) had 101 patients and arm B (control arm treated with oral anticoagulant and ECS) had 108 patients. The primary endpoint of the trial was the frequency of post-thrombotic syndrome after 24 months of follow-up.
Of the 90 CDT-treated patients and 99 control patients who had data available for analysis, 41.1% of patients treated with CDT presented symptoms of post-thrombotic syndrome compared to 55.6% of control patients. The difference in post-thrombotic syndrome incidence corresponds to an absolute risk reduction of 14.4% in patients treated with CDT.
Twenty bleeding complications were reported, three classified as major and five considered clinically relevant. None of the reported bleeding episodes caused serious complications, and there were no pulmonary emboli, strokes, or deaths related to treatment with CDT. After six months of follow-up, post-thrombotic syndrome developed in 36.9% of patients who no longer had a clotted vein, as compared to 61.3% of patients who still experienced clotting. These outcomes underscore the importance of recanalisation for preventing post-thrombotic syndrome and ensuring positive outcomes in patients with deep vein thrombosis.
“The results of our trial show that additional treatment with CDT significantly reduces the risk of post-thrombotic syndrome in patients with DVT, compared to standard treatment alone,” said Per Morten Sandset, senior author and Head of Research, Clinic of Cancer, Surgery, and Transplantation, Oslo University Hospital, Norway. “Although CDT is a promising treatment option for patients with iliofemoral DVT, the therapy also increases the risk of bleeding, emphasising the importance of patient selection and safety when performing CDT procedures. Our findings suggest that CDT should be considered in patients with upper thigh or pelvic DVT.”