In a new study presented at the American College of Cardiology 66th Annual Scientific Session, researchers from the Perelman School of Medicine at the University of Pennsylvania have found that the utilisation rates of these potentially life-saving medications are low, particularly in the sub-group of pulmonary embolism patients who are critically ill.
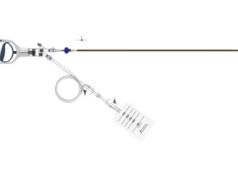
Systemic thrombolysis is the method in which “clot-busting” medication is administered intravenously (IV) to eliminate clots throughout the bloodstream, while catheter-directed thrombolysis allows the medication to be directly administered into the clot in the lungs.
“For years, systemic thrombolysis and catheter-directed thrombolysis have been available for use in patients with pulmonary embolism, however, there has been little research done to understand how these therapies are being utilised in the real-world,” said the study’s presenter Srinath Adusumalli, chief cardiovascular medicine fellow in the Perelman School of Medicine at the University of Pennsylvania, USA. “Our initial data suggest that, in fact, both systemic thrombolysis and catheter-directed thrombolysis are used infrequently to treat pulmonary embolism, including in young, critically ill patients who may experience the highest clinical benefit from those therapies.”
Adusumalli and colleagues performed a retrospective study in which they collected data from the OptumInsight national commercial insurance claims database and identified 100,744 patients who had been hospitalised with pulmonary embolism during a ten-year period (2004–2014). This is the first study of its kind to examine detailed procedural coding for pulmonary embolism therapies from a national database, allowing researchers to aggregate information from a national population rather than hospital or region-specific information. The team culled through the data and found that of the 100,744 patients hospitalised with pulmonary embolism, 2,175 patients received either catheter-directed thrombolysis or systemic thrombolysis—roughly 2% of all pulmonary embolism patients. In this same timeframe, the number of pulmonary embolism hospitalisations increased by 306%.
“Another question that emerged from these findings is whether we are adequately matching the right patients to the right therapies at the right time,” said senior author Peter W Groeneveld, an associate professor of Medicine, research director in the Leonard Davis Institute of Health Economics, and director of Penn’s Cardiovascular Outcomes, Quality, and Evaluative Research Center, USA. “Since there is a lack of real-world clinical effectiveness and safety data on these therapies and a resulting lack of guideline-based recommendations, substantial clinical uncertainty persists as to when and in whom to use catheter-directed thrombolysis and systemic thrombolysis.”
A larger team at Penn Medicine, including those who were involved with this study, created what’s called the Pulmonary Embolism Response Team—PERT—which is designed to employ rapid response techniques for the treatment of pulmonary embolism in order to match the right patient to the right therapy at the right time.
“The purpose of PERT is to ensure that high-risk pulmonary embolism patients are receiving the best kind of treatment plan on the most efficient timeline in order to improve outcomes,” said Jay Giri, an assistant professor of Cardiovascular Medicine and founder of the PERT at the Hospital of the University of Pennsylvania. “However, it is important to state that most decisions made by PERT physicians are a matter of clinical consensus rather than being based on rigorous comparative effectiveness research. The current study re-emphasises the clinical consequences of the dearth of data in the pulmonary embolism field.”
While the team notes these data are clinically useful and could impact the patient care decision-making process, there is still more research needed. Co-presenter and study author Bram Geller a cardiovascular medicine fellow in the Perelman School of Medicine at the University of Pennsylvania, added, “This study is the first in a two-step research plan, in which our next phase will be to actually evaluate the safety and clinical effectiveness of catheter-directed thrombolysis versus systemic thrombolysis by exploring patient outcomes in the OptumInsight commercial insurance claims database.”