As course director of The VEINS at VIVA 2019 (2–4 November, Las Vegas, USA), John Kaufman tells Venous News how the field of interventional radiology (IR) has transformed over the years and highlights key areas of innovation to look out for in the future.
What inspired you to enter the field of medicine and how did you first become interested in interventional radiology as a specialty?
I went in to both medicine and radiology because of my father, Seymour Kaufman. He trained during World War II in an accelerated US Army programme; remarkably, he had his MD by the age of 21. He really loved what he did, and in high-school I would develop X-rays for him in his office on Saturdays. Radiology and interventional radiology took a little longer to figure out—I was a rebel so I started in surgery. Over time I realised that my father was smarter than I had thought, and radiology was the way to go. In my first year of diagnostic residency I rotated onto “Special Procedures” with the late, brilliant Alan Greenfield. He started me on the path to IR and I never looked back.
As a trainee doctor, which figures in the IR field were some of your key mentors?
I think almost everyone I have interacted with in this specialty has given me something that I still carry today. Patients, fellows, nurses, technologists, support staff, administrators, physician colleagues (from IR and other specialties), professional society staff, and many industry partners have all mentored me in their own ways. Everyone has something to teach you. Some who stand out as having been particularly tolerant of me are Alan Greenfield, John Guben, Jim Parker, Michael Bettmann, Greg Walker, Stuart Geller, Arthur Waltman, Jan Durham, Peter Mueller, Kathy Krol, Barry Katzen, Gary Becker, Josef Rosch, Fred Keller, Matt Mauro, and Anne Roberts. But there are many, many more.
During your time as an interventional radiologist, what have been some of the major changes to the field and how has this impacted upon your practice?
I have been doing this long enough that my answer includes the availability of such common technologies (today) as stents, microcatheters, volumetric CT, and high-resolution digital subtraction angiography (DSA). However, I think the biggest changes have not been the new technologies. The first major change is that image-guided procedures have become mainstream, such that medicine without them is now inconceivable. Take the Transjugular intrahepatic portosystemic shunt (TIPS) procedure for complications of portal hypertension, developed by Josef Rosch from my institution; modern hepatology cannot function without it. The second major change is the broad application of the scientific method when bringing new technologies and procedures forward. Although the process is now slower than in the past, it is the right way to move ahead. The third is the recognition that the patient is the focus, not the technology or the physician or their specialty. The validation of image-guided interventions has led to adoption by many specialties that are all equally dedicated to their patients. We can all work together for the common goal of improving patient outcomes. This the core principle behind all that we do at VIVA, and I hope one that all specialties will ultimately embrace.
How great a challenge was it to gain recognition for IR as a primary specialty in the USA?
Change is a fascinating process in general, and always seems more obvious in retrospect. The transition from sub-specialty of diagnostic radiology (DR) to a primary specialty followed many of the classic steps of implementing major changes; refinement of the message, initial champions, engagement of key stakeholders, early adopters, and all that follows. Many of the challenges were internal to IR and DR as would be expected, and these were the most important to address up front. It is really hard to convince the American Board of Medical Specialties (ABMS) that something is a legitimate primary specialty, and that the benefit to patients outweighs all of the logistical, bureaucratic, and economic burdens that specialty status imposes upon society. In the end, it was the support of all but one ABMS specialty that encouraged us to bring this to fruition. The immense popularity of the new IR residencies and the high quality of the candidates has been very gratifying to see.
What made you decide to move across the country—from Harvard Medical School to Portland, Oregon—after spending so much of your personal and professional life in Boston?
The Dotter Institute and the Pacific Northwest. For me, it was a great professional move in terms of the people, history, and potential here, and it just gets better every year. For our family, it matched our interests and lifestyle. We do miss being closer to family, but my wife has never looked back!
What are some of the key areas of innovation and research that you are keeping an eye on, especially in your role as editor for the American Journal of Radiology?
We are all watching machine learning and artificial intelligence (AI) with intense interest. On the face of it, one might assume that proceduralists may be less impacted than imagers, but AI will become integral to our decision making processes before, during, and after interventions. It is less likely that computers will do the actual procedures; instead, they will analyse images, laboratory results, and symptoms. That being said, we will rely on AI for vast segments of our non-procedural practice. Another area that we should all be watching closely is outcomes research. Proving that image-guided procedures provide better outcomes at less expense and with higher patient acceptance than traditional open procedures requires solid scientific work. The recent controversy over paclitaxel is just one example of how easy it is to focus on the outcomes that interest us the most. In the venous world, we will need to prove that all of the stents that we are now placing lead to improved outcomes.
As course director of The VEINS at VIVA, what are you looking forward to most at this year’s event?
The VEINS at VIVA meeting is even bigger this year than last. Raghu Kolluri is literally a force of nature, and the result is a great programme with high-level speakers that covers the full spectrum of venous diseases. This year we have added an all-star multidisciplinary scientific committee—including Suman Wasan, Suresh Vedantham, and Lowell Kabnick—who have enhanced the content tremendously. But to answer your question, what I am looking forward to most is learning a lot.
Are there any especially memorable cases which stand out to you from your time as an interventional radiologist?
We all cherish the saves—the patients that we somehow pull back from the brink. I also think a lot about those that I have lost, or somehow failed. I feel that I owe it to them to not forget; if there can be any good in their sacrifices, it is trying not to let it happen again. Finally, I really enjoy the patients that I work with over time who I get to know as people, rather than conditions or diseases. This is the truly magical side of IR.
Could you describe the proudest moment of your career?
That is easy: any time I am called out as the father of Claire Kaufman, MD. That supplanted hanging my medical school diploma on the wall next to my father’s. It is fantastic, truly awesome, and she is going to make me look like a back-bencher.
If you could give any advice to a new IR specialist graduating from medical school today, what would you say?
The best part of image-guided interventions is yet to come. Keep an open mind, think beyond the lesion, and collaborate. This space is going to remain one of the most exciting, innovative aspects of medicine for a long time. Much of what you learn and do when you graduate will be replaced with new procedures within 10 years; most of which you cannot even imagine right now. This is hard work, but it is worth it!
What are some of your hobbies and interests outside of medicine?
This will be a pathetically short answer—my continually expanding family of people and dogs, cooking (especially long complicated recipes that involve pasta), good wine, and more recently roasting coffee. I would also fly-fish if I could find the time.
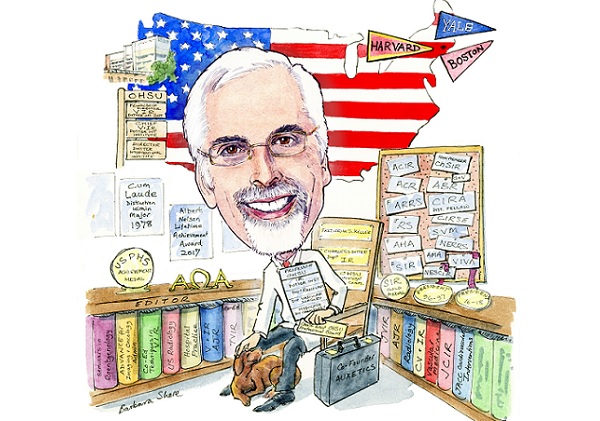
Fact File:
Qualifications:
1978 BA, Yale University
1982 MD, Boston University School of Medicine
2010 MS, Harvard School of Public Health
Academic Appointments (selected):
1997–2000 Associate professor of radiology, Harvard Medical School
2000–Present Professor of interventional radiology, Dotter Interventional Institute, Oregon Health & Sciences University
2003–Present Professor of surgery, Division of Vascular Surgery, Oregon Health & Sciences University
2005-Present Frederick S. Keller endowed chair of interventional radiology, Dotter Interventional Institute, Oregon Health & Sciences University
Professional Appointments (selected):
1983–1985 General medical officer and director of emergency medical services, W.W. Hastings Indian Hospital
1998–2000 Fellowship director, vascular/ interventional radiology, Massachusetts General Hospital
2003–Present Chief of vascular and interventional radiology, Dotter Interventional Institute, Oregon Health & Sciences University
2012–Present Director, Dotter Interventional Institute, Oregon Health & Sciences University
2017–Present Chair, Charles T. Dotter Department of Interventional Radiology
Offices (selected):
2003–2005 Chair, Council on Cardiovascular Radiology and Intervention, American Heart Association (AHA)
2008–2009 President, Society of Interventional Radiology (SIR)
2016-2018 President, VIVA Physicians
2018–Present Governor, American Board of Radiology









