The new Crux inferior vena cava filter can be implanted and retrieved safely and shows a low rate of pulmonary embolism, Anthony J Comerota, director, Jobst Vascular Institute, adjunct professor of Surgery, University of Michigan, USA, told delegates at the Vascular Annual Meeting (7–9 June 2012). He spoke about new developments with inferior vena cava filters at the conference in National Harbor, USA.
Comerota noted that the second randomised trial with inferior vena cava filters was performed by investigators from the Maimonides Medical Center, Brooklyn, New York. In the trial (Usoh et al. J Vasc Surg 2010), 156 patients were randomised to the Greenfield (Boston Scientific) or TrapEase (Cordis) filters.
The study was stopped at the interim analysis stage because, at 12 months, the symptomatic vena cava occlusion rate was 7% in the TrapEase group vs. 0% in the Greenfield group (p=0.019). “Therefore, the IRB [institutional review board] thought it was unethical to continue the trial,” Comerota said. “This study showed that double conical filters are associated with unacceptable high rates of venal cava occlusion.”
Comerota also commented on the results of the Systematic Review of the Use of Retrievable Inferior Vena Cava Filters, by Angel et al (J Vasc Interven Radiol 2011).
“This is the most robust look at retrievable inferior vena cava filters. It included a Medline search for 37 studies comprising 6,834 patients. It did not include randomised trials but there were 11 studies thought to be of high suitability. What they found in data from 6,834 filters was that 58% were used without any underlying pulmonary embolism or deep venous thrombosis, the traditional prophylactic use; 70% were inserted via the femoral vein, but interestingly there were no reports of placement complications. The mean follow-up was less than 10 months, which is a shortcome,” Comerota said.
He added that the rate of pulmonary embolism in the high suitability studies was 2%; deep vein thrombosis was reported in 5.4% of the cases and the rate of vena cava thrombosis was 2.8%. Migration and filter fracture occurred predominantly in the G2 filter (Bard).
“Retrieval occurred in only 34% of these retrievable inferior vena cava filters, with a mean time of 72 days. But when attempts were made within three months, retrieval success was over 90%. When retrieval was attempted at 12 months the success rate dropped dramatically to 37%. Overall, the retrieval failure rate was 5.5%. ‘Lost to follow-up’ was the most common reason for non-retrieval,” he said. “The conclusion was that ‘in high-risk patients for whom anticoagulation is not feasible, retrievable inferior vena cava filters seem effective in preventing pulmonary embolism, but that long-term complications are a serious concern’.
“So is there a problem with not removing a retrievable inferior vena cava filter? The FDA believes there is. To date, there have been over 1,000 reported device adverse events, and the FDA strongly states that with retrievable inferior vena cava filters, we need to consider removing the filter as soon as protection from pulmonary embolism is no longer needed,” he said. “This systematic review shows that retrievable filters are effective in the short term, but there are serious concerns with long-term complications.”
After that, Comerota discussed the results of what he considers to be “the most important study published in a number of years on pulmonary embolism and inferior vena cava filters”. The study by Stein et al (Am J Med 2012; 125:478-484) aimed to determine categories of patients with pulmonary embolism in whom vena cava filters reduce in-hospital case-fatality rate. Using the Nationwide Inpatient Sample (1999–2008), the investigators analysed more than 2 million patients.
“They found that there was a significant reduction in mortality in patients with pulmonary embolism who received an inferior vena cava filter. Independently of whether they were stable and not receiving lytics, stable and receiving lytics, unstable and receiving lytics or unstable patients, they all had a reduction in mortality. The only subgroup that did not fare well with the filter comprised stable patients with pulmonary embolism with an associated deep vein thrombosis group (6.7% with filter vs. 5.3% with no filter, p<0.0001). To me this is counter-intuitive but the number was 721,200 so it is a robust denominator,” Comerota said.
“In general, we can see that those stable patients who received lytic therapy or unstable patients may well benefit in a reduction in mortality by receiving an inferior vena cava filter. The number needed to treat is 11 or less, which is a very high return on your investment. So the conclusion was that it does seem to be prudent to consider inferior vena cava filters in pulmonary embolism patients who are going to have thrombolytic therapy or who are unstable.”
Comerota concluded the talk analysing the results of the Crux filter from Crux Biomedical.
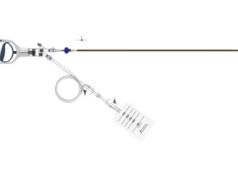
“I think the Crux device, with a brand new design, is the most innovative development in inferior vena cava filters. The clinical trial has just been completed, and the data have been submitted to the FDA. The device has a helical design, with a nitinol wire frame, and the filtering is due to extruded polytetrafluoroethylene (ePTFE),” he described.
One hundred and twenty five patients (58% male, mean age 59 years) were enrolled in the multicentre, single-arm study and followed up for 180 days. The indications for filter placement were surgical risk for pulmonary embolism in 36% of the cases and contraindication to anticoagulation in 37%.
Technical success with the device was 98%. Deployment time was five minutes and retrieval time was seven minutes. Retrieval success was 98% at a mean of 84 days. “Retrieval and placement can be obtained both from the jugular and the femoral approach,” Comerota said.
Fifty seven per cent of the patients had the filter remaining in place as permanent. Pulmonary embolism was observed in 2.4%. He added, “However, there was no filter migration, embolisation, fracture or tilting.” He concluded that the device “can be implanted and retrieved safely with a very high success rate and a low rate of pulmonary embolism.”
The Crux inferior vena cava filter was cleared by the FDA in July.