
At the European Society of Vascular Surgery annual meeting (ESVS 2019; 24-27 September, Hamburg, Germany), preliminary venous thrombosis guidelines were presented for the first time. Chaired by Stavros Kakkos (Patras, Greece) and Manj Gohel (Cambridge University Hospitals, Cambridge, UK), and supported by an international writing group comprising of recognised thrombosis experts, the finalised guidelines will be published in 2020 and add to the list of ESVS treatment guidelines for a range of arterial and venous disorders.
In recent years, the venous field has witnessed a considerable number of advances, and a range of new evidence, on thrombosis. The guideline writing committee, which was comprised of a wide variety of medical professionals, represented the diverse range of specialities involved in the management of venous thrombosis internationally. Previous thrombosis guidelines, such as those published by the American College of Chest Physicians (ACCP) or the American Society of Haematology (ASH) have provided important support for clinical teams. However, several common and challenging areas are not extensively covered in these publications.
One important area extensively covered in the ESVS guidelines is the management of superficial vein thrombosis (SVT), also known as thrombophlebitis. Patients with SVT are frequently referred to acute thrombosis services, primarily to exclude the more serious differential of deep vein thrombosis (DVT). However, the true importance and potentially serious complications of SVT have not been well-appreciated. Several studies have demonstrated that SVT is associated with a high risk of recurrence, progression to DVT or pulmonary embolism (PE), particularly in the first three months. Overall, there is a greater appreciation that SVT is not the benign entity that many clinicians have traditionally perceived it to be.
Important randomised clinical trials have highlighted the importance of whole leg ultrasound assessment to provide detailed information of the site and extent of the venous thrombosis. On the basis of ultrasound assessment, risk stratification can be performed, guiding targeted anticoagulation therapy to reduce the risk of progression to DVT or PE. The vast majority of patients with SVT have superficial venous reflux and associated venous stasis. Moreover, an area of great controversy is the role and timing of superficial venous ablation in patients with SVT.
Traditionally, some patients have been managed with expedited surgical ligation of saphenofemoral or saphenopopliteal junctions, to eliminate the risk of thrombus progression into the deep system. However, the more widespread evidence for the use of anticoagulation has largely eliminated the need for any acute venous intervention. Repeat duplex ultrasound imaging and deferred intervention is probably justified for the majority of patients. Any superficial venous intervention during the period of acute inflammation is likely to be associated with a higher risk of peri-procedural venous thromboembolism.
Despite the enormous volume of published venous research, there remain several areas with just a few high quality (and no randomised) clinical trials. Such conditions present a huge challenge to guideline writing committees, particularly when the condition is common. One such area is the management of upper extremity venous thrombosis. Less common than lower extremity DVT, upper extremity thrombosis is most commonly associated with intravenous catheters. However, the management of ‘effort thrombosis’, also known as Paget Schröetter syndrome, is particularly controversial. Enormous variations exist in clinical care, ranging from conservative management with anticoagulation alone, to a much more aggressive approach involving early thrombus removal, with prompt first rib resection to decompress the thoracic outlet.
In the absence of randomised trials, the committee relied on non-randomised evidence from observational studies and many of the recommendations are likely to have been extrapolated from studies of lower extremity DVT. While aggressive thrombus removal may be justified in some individuals, anticoagulation alone is likely to be adequate for the majority of patients with upper extremity DVT.
When considering the use of early thrombus removal for patients with acute iliofemoral and femoropopliteal DVT, the ATTRACT trial has resulted in considerable controversy and debate. The primary outcome results failed to demonstrate a significant benefit for early thrombus removal strategies over anticoagulation alone. A subsequent analysis, including only patients with iliofemoral DVT, did suggest that moderate-to-severe post-thrombotic syndrome (PTS) may be prevented in a subset of patients treated with aggressive thrombus removal. The real challenge remains patient selection, as most patients with acute iliofemoral DVT do not develop significant PTS when managed with anticoagulation alone. Additional areas of uncertainty are the indications and role of stenting after early thrombus removal, the optimal modality for thrombus removal and the ideal post-intervention anticoagulation policy. While there may be some evidence to suggest that more technically successful thrombus removal may yield greater clinical benefits, the best approach to reach this goal is unclear.
One novel area covered in detail, as part of the 2020 venous thrombosis guidelines presented at ESVS 2019, will be the use of compression therapy in the acute and later phase after lower extremity DVT. There remains a general reluctance to initiate compression therapy for patients immediately after diagnosis of acute DVT, possibly due to concerns about pain, patient compliance or fears over pulmonary emboli. However, several randomised trials have demonstrated the clear benefits of compression therapy in the acute phase to alleviate symptoms of pain and oedema, and reducing residual vein obstruction. Extended use of compression has been the subject of several randomised trials, with most demonstrating a beneficial effect in reducing the risk of post-thrombotic syndrome at 24 months with the use of compression stockings.
The recent IDEAL DVT study further advanced our understanding by demonstrating that patients wearing stockings after acute DVT and with few symptoms (evaluated by Villalta score) can discontinue stockings after six or 12 months, and without any increase in PTS risk at 24 months. This evidence empowers clinical teams to better customise treatment duration to individual patients, avoiding the cost and inconvenience of prolonged use of compression where is it unnecessary. More widespread use of compression, including in the acute phase after diagnosis of DVT is likely to be a relatively easy and cheap intervention to improve patient symptoms and quality of life.
The guidelines will also cover a range of other key areas: the treatment of calf vein thrombosis, type and duration of anticoagulation therapy after provoked and unprovoked DVT, surveillance after DVT, indications and use of inferior vena cava (IVC) filters, catheter-related thrombosis and a range of special patient populations include pregnant patients and those with inherited or acquired thrombophilia. It should be recognised that there remain many areas within venous thrombosis where the quantity and quality of available evidence is poor.
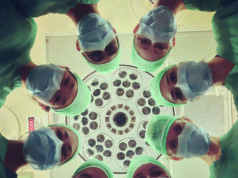
While there have been advances in the evidence base, many questions remain, most notably how to best select the patients most likely to benefit from the plethora of effective interventions that are now available. Despite these uncertainties, it is clear that health professionals from a wide array of medical and surgical specialities have an important role to play. Haematologists, vascular surgeons, angiologists, internal medicine specialists and others have to work in close collaboration to share experience and skills. Only then do we stand a chance of addressing the outstanding areas of uncertainty in the management of venous thrombosis.
Manj Gohel is a consultant vascular and endovascular surgeon at Cambridge University Hospitals, Cambridge, UK.









Very interesting and controversial subject.
I agree that there is un underestimation of this pathology and it is a great mistake beacause a superficial thrombophlebitis can hide a thrombophilia or a cancer, besides the possibility of a TEP.
I believe that we should act following an algorhytm diagnosis to prevent conplications.