This advertorial is sponsored by Optimed.

Before the STEVECO trial, there were no randomized controlled trial data in the chronic disease space; in its wake, has come a more robust landscape to establish an evidence base: During the 2024 Charing Cross (CX) International Symposium (April 23–25, London, UK), Stephen Black (Guy’s and St Thomas’ NHS Foundation Trust and King’s College London, London, UK), Efthymios Avgerinos (Athens Medical Center and University of Athens, Greece), and Erin Murphy (Atrium Health’s Sanger Heart and Vascular Institute, Charlotte, USA) sat down with Houman Jalaie (University Hospital RWTH, Aachen, Germany), to discuss the STEVECO trial and how it provides necessary data on venous stenting for patients affected by chronic venous insufficiency.
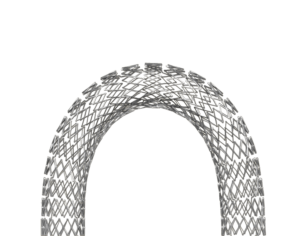
The STEVECO (Stent versus conservative treatment in patients with deep venous obstruction) trial is a prospective, randomized, multicenter, 12-month trial comparing venous stenting using Optimed’s sinus-Venous stent to conservative treatment. The trial measured disease-specific quality of life (QoL), Venous Clinical Severity Score (VCSS), and patency in 63 patients who had either post-thrombotic syndrome (PTS) or non-thrombotic iliac vein lesions (NIVLs). The results of the study showed that symptomatic patients with deep venous obstruction who received the sinus-Venous dedicated venous stent had significant improvement in QoL after 12 months. There was also a significant improvement in VCSS and the pain disability index.
To begin the roundtable discussion, Jalaie, senior author for the STEVECO trial, asked Black what the next steps are for bringing more evidence to the venous stenting field.
“That’s a great question,” Black said. “Obviously, you and your team have to be congratulated on performing this trial because there has been no randomized data in the chronic space before STEVECO, and I know the difficulties you had with running it. We need data of some description, we need bigger registry data, and we work here on a project with the European Society for Vascular Surgery (ESVS) and the Cardiovascular and Interventional Radiological Society of Europe (CIRSE) to set up a European registry.”
Black praised the STEVECO trial, saying that it helps to establish more robust databases to support therapies that the vascular community is trying to offer patients.
Jalaie then turned his focus to Avgerinos, asking “what about Europe-wide efforts in terms of registries to augment the evidence base for venous stenting?”
“It’s an exciting time for the venous world, it’s an exciting time for ESVS,” Avgerinos said. “As we’re launching the ESVS venous registry, we’re going to get vein centers all around Europe to start entering data on deep venous intervention. We are also involving CIRSE to make sure that we get all the specialties in.”
Avgerinos continued, saying that one of other major goals of this registry is to help better assess the efficiency of venous procedures and the long-term follow-up that randomized controlled trials cannot currently give.
“The current ESVS guidelines on chronic venous disease were published in 2022,” Avgerinos stated. “That was just a little bit before the STEVECO trial came out, so it does not include the STEVECO trial. The guidelines right now include the fact that we can stent patients with iliac vein outflow obstruction when they have severe symptoms.” Avgerinos believes that adding the knowledge from the STEVECO trial will help upgrade the level of evidence for chronic venous disease from a B to an A.
“I think this will embark on a new era in the management of patients with post-thrombotic syndrome,” Avgerinos said.
Jalaie asked Murphy what could be done better in the future when it comes to patient recruitment, as the STEVECO trial struggled there.
Murphy responded, “Recruiting participants for randomized controlled trials has proven challenging, as we’ve seen across multiple studies. While there is a demand for high-grade evidence, we need to consider whether additional randomized controlled trials are necessary. We now have the STEVECO data, extensive data sets from IDE stent trials, and numerous smaller single-center trials, all consistently showing that venous stenting is effective across patient subgroups. These studies universally demonstrate improvements in quality of life and venous functional outcome scores.”
Murphy continued, “I believe our next step should be trials focusing on real-world data across various specialties treating these patients. We need data that offers more insights into patient selection, identifying which patients benefit the most, and finding ways to reduce risks for higher-risk post-thrombotic patients.”
Black went even further, discussing how recruitment has plagued nearly every trial in the venous space. He specifically mentioned the C-TRACT trial and the UK-based BEST-PTS trial, the latter of which was suspended due to recruitment issues.
“STEVECO was helpful in revising recruitment targets,” Black said. “Because the data from your study allowed us to drop the numbers that we needed to recruit.”
“Probably the way to address recruitment is to look at novel trial designs that do not involve randomization of patients to try and get everybody into some form of prospective data collection,” Black continued. “Registries have their limitations, of course, but there are other options for trial design, particularly in the era of artificial intelligence (AI) that are now coming to the fore, which allow you to enroll everybody regardless of treatment or place.”
Murphy emphasized the importance of standardizing data collection across trials, stating, “We need to ensure consistency in what we’re collecting. In reviewing those IDE trials, it became evident that they examined different patient groups and thought they were looking at the same conditions—PTS and NIVL—but the definitions varied across the trials.”
“I hope that we can get to a more standardized approach,” Black responded. “We’ve been trying on several different fronts to make sure that people are reporting to standard outcome measures.”
“When you touch again on aspects of all the trials that need to be optimized, if we do a trial of a technique that involves technical skill, ability, and a learning curve, and don’t do it when people have optimized how they deliver that treatment, you’re going to get a trial of a poor intervention against doing nothing, which is unlikely to give an outcome that is beneficial to patients or us,” Black added. “Technical success delivers optimal outcomes to the patients.”
When it comes to using technical tools to help select patients, Avgerinos says that above all else, the patient’s anatomy must be known.
“To be well prepared, to intervene, and to better communicate with our patients, we need to have good imaging,” Avgerinos said. “In today’s practice, I think imaging techniques have evolved.”
Avgerinos continued the conversation, explaining that while magnetic resonance venography (MRV) and computed-tomography venograms (CTV) are good, intravascular ultrasound (IVUS) will give the best imaging results. By combining IVUS with duplex and axial imaging, he said, you can decide which patients will benefit the most from specific procedures.
Moving towards the treatment of younger patients, Jalaie asked “How do we make sure to provide the best longterm treatment?”
Black answered first, stating that the stents patients receive need to be durable, especially in female patients who may, in the future, want to have children.
“We need to see the long-term durability for these treatments,” Black said. “Of course, we can only get that once these stents have been in people for a long time, so some of it has to be predicted.”
“We also have to work on the things that we’ve forgotten about in the drama around what is the next stent,” Black continued. “We need to maintain stents in patients and look after them. That comes with better drug therapy, potentially innovation around technologies that help us to look after stents for the lifetime of a patient, and we need to optimize that implantation phase of that stent.
Avgerinos spoke about anticoagulation, noting that there aren’t robust data regarding it, but “from what we know it seems that low molecular weight heparin, with its anti-inflammatory effects, may be beneficial in the early period after placing a stent.”
The roundtable discussion closed out with Jalaie asking the panel whether or not these procedures should be centralized.
“You have to do enough and do them often enough to become good, and that’s in the best interest of patients,” Black concluded. “Hopefully the data that we’re all generating can support that narrative as it has done for aortic surgery in the past.”
sinus-Venous is not for sale in the USA.









