The use of ultrasound-accelerated catheter-directed thrombolysis to treat acute iliofemoral deep vein thrombosis continues to be feasible and safe, according to a study presented by Rob H W Strijkers (Department of Vascular Surgery and Cardiovascular Research Institute Masstricht, Maastricht University, Limburg, The Netherlands) at the 13th Meeting of the European Venous Forum (Florence, Italy, 28-30 June 2012).
Previous positive results on the Maastricht and Aachen clinical experience were presented by Strijkers at the European Venous Forum in Ljubljna, Slovenia, last year.
According to Kahn et al, Strijkers said, “Iliofemoral vein thrombosis is associated with a twofold increased risk of developing post-thrombotic syndrome.” However, “early thrombolysis may decrease the incidence of this syndrome,” Strijkers noted. “Results presented from the CaVent study, in December last year, showed an absolute risk reduction of 14.4% in the incidence of post-thrombotic syndrome in patients with iliofemoral deep vein thrombosis treated with catheter-directed thrombolysis.”
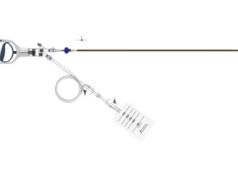
Strijkers highlighted that new catheters with mechanical components such as the Ekos endowave system (used in this study), Trellis-8 or the Angiojet system may enhance clot lysis and lower treatment time and bleeding complications.
At this year’s meeting, Strijkers presented data of patients with acute iliofemoral deep vein thrombosis treated with ultrasound-accelerated catheter-directed thrombolysis, from October 2008 to March 2012. Cases with in-stent thrombosis and chronic clots, which are also part of the Maastricht and Aachen clinical experience, were excluded.
The main outcome of the study was patency at one year. Secondary outcomes included: treatment time, bleeding complications, and pulmonary embolism. Diagnosis of deep vein thrombosis was assessed using duplex sonography and/or magnetic resonance venography and CT venography.
In the study, 37 patients, average age 42 years (5–76), were included. The deep venous thrombosis location was unilateral in 33 patients (20 left side, 13 right) and bilateral in four patients. The average treatment duration was 43 hours, success rate of recanalisation was 95% (n=35) and re-thrombosis occurred after 11 (30%) procedures. Additional procedures of underlying stenotic disease were required in 18 patients.
Strijkers highlighted that there were no cases of major bleeding and only three patients had minor bleeding at the insertion point of the catheter. One case of pulmonary embolism was reported and one additional complication due to prolonged catheter placement was observed. There were no intracranial haemorrhages cases and no deaths related to treatment.
Strijkers told delegates that one year patency results are reasonable with 70% patency rate and secondary patency of 87% after one year.
Looking at the future of thrombus removal, Strijkers told delegates that there are two randomised controlled trials currently recruiting patients: the ATTRACT trial in USA and the CAVA trial in The Netherlands, which incorporate clinical endpoints such as post-thrombotic syndrome and quality of life. “We think that with these studies, together with the CaVent study, we can report critical evidence in the treatment of patients with deep vein thrombosis.”