At the recent 6th SITE meeting on Endovascular Therapeutics in Barcelona, Spain. Dr Attilio Cavezzi of the Clinica Stella Maris, S.Benedetto del Tronto, Italy, presented the latest research in foam sclerotherapy. The objective of his study was to describe the main stages of the technique and the latest advancements in (duplex guided) foam sclerotherapy (DGFS).
Foam sclerotherapy (SF) uses a mixture of air and detergent solution to produce bubbles, which are injected into veins. Since 2002 Cavezzi and his research team have introduced and studied several adjuvant measures to increase efficacy and safety of the treatment. The procedures include:
Cavezzi and his research team also studied a combined surgery-sclerotherapy procedure, which resulted in a quicker achievement of the end-point with usage of low concentration and doses of STS or POL and lower rate of varicophlebitis-pigmentation. He said the mid-term follow-up compared favourably with their personal outcomes of single DGFS or phlebectomy, as well as with literature data about standard saphenous stripping.
The presence of a competent terminal valve at the saphenofemoral or saphenopopliteal junction has proved a favourable factor for the mid-term outcomes, Cavezzi said, as well as smaller vein calibres better responding to DGFS.
The researchers concluded that the new research findings and concepts of other authors can reasonably improve the efficacy and safety of foam sclerotherapy. Cavezzi said a certain degree of standardisation in the management and in the indications of foam sclerotherapy has been agreed, although several variables are still recognised. He added that studies with larger series and with longer follow-up are needed in the close future to assess properly the safety and efficacy of foam sclerotherapy.
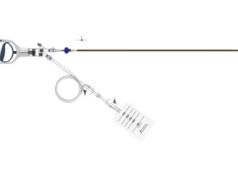
At the 2005 Ajaccio workshop, Dr Michel Perrin, Vascular Surgery, Lyon, France, presented a literature review of techniques for endovenous treatment of varicose veins (VV), namely Endovenous Laser (EVL) and Radiofrequency (RF). He began by stating that EVL and Radiofrequency have been the subject of numerous publications during recent years. The presentation analysed a number of articles published in English (n=53) and French (n=20) and compared the two procedures with each other and with classical surgery. While RF uses only one type of device manufactured and distributed by a sole company, EVL uses different types of lasers, manufactured and marketed by several companies. Therefore, RF benefits from a well-defined procedural protocol, in contrast to EVL, which presents multiple variants.
The results showed that the short-term and two years post-operative clinical status were studied in two controlled randomised trials comparing RF with classical surgery including one study that used a quality of life questionnaire. The results, including return to normal activity and duration of convalescence, were more favourable after RF. In terms of thromboembolic complications investigated by systematic Duplex ultrasound (DU) examination, the two procedures presented an approximately equal rate of 0.5%. Other post-operative complications were transient: RF has been associated with sensory nerve complications like paresthesia, while pain was more pronounced after EVL. Perrin said the results were difficult to analyze in terms of varicose vein treatment. In terms of signs and symptoms, detailed results were available at four years follow-up for RF.
The improvement was very significant compared to the pre-operative status and roughly equivalent to that previously reported for classical surgery. Clinical results after EVL are less documented. Haemodynamic results by duplex ultrasound examination are well documented for RF but less detailed for EVL. In a single center study, vein obliteration after EVL is 96.8% at two years follow-up (31 limbs); vein obliteration is 88.8% after RF in a multi-centre study (98 limbs) and varicose vein recurrence 21.4 % at four years follow-up.
Correlation between clinical and haemodynamic results was established for RF at two years follow-up and showed a strong link between the clinical results and absence of reflux. Finally, the cost estimation of the two techniques showed that the EVL fibre is cheaper than the RF catheter, the situation being the inverse for the generators. The global cost of the RF procedure (including convalescence) was compared to classical surgery in a study. The findings favour RF for active patients.
Perrin claims the review highlights the absence of phenomena of neovascularisation, in particular at the saphenofemoral junction following endoluminal surgery. It is known that this phenomenon, which occurs frequently, from 20-40 % at five years after conventional surgery plays an important role in the incidence of recurrence. It is difficult to determine whether or not using high ligation in endovenous procedure can alone explain the absence of neovascularisation. However, Perrin claims that it is possible that maintaining the patency of the saphenous termination tributaries plays a favourable role in that they drain physiologically, as shown in duplex ultrasound investigation performed at two years after great saphenous vein RF endovenous obliteration. In addition, the incidence of postoperative deep vein thrombosis assessed with systematic post operative duplex ultrasound is comparable to the one provided by classical surgery. In a recent study the incidence of postoperative deep vein thrombosis after high ligation stripping was 5.3 %.
Nevertheless, Perrin stated that some vascular surgeons are reluctant to use these new promising VV endovenous treatments and remain persuaded that interventional treatment without high ligation is a crime of lese-majesty. Perrin said that this assertion is not correct as several DUPLEX ULTRASOUND studies have shown that in about 50 to 70 % of patients with incompetence of the saphenous trunk, the saphenous terminal valve is competent. This means that the saphenofemoral or saphenopopliteal junction does not need to be resected. Besides, when the terminal valve is refluxive, endoluminal treatment by shrinking the venous lumen possibly restores the valve competence as shown by postoperative US investigation. “To convince them we need prospective studies in which the terminal and the subterminal valves should be preoperatively, precisely assessed in order to know if the results are significantly different when the terminal valve is incompetent or not. That will clarify indication for using endoluminal treatment,” Perrin said.
Perrin concluded that in the absence of long term controlled results (beyond five years) comparing classical surgery to endoluminal surgery, the latter method was proven to be less aggressive post-operatively and effective at mid-term. The suppression of the saphenous vein reflux exhibits an enduplex ultrasoundring treatment efficacy clinically, anatomically and haemodynamically up to four years for RF and two years for EVL.
At the 12th Ajaccio workshop Dr Thomas Proebstle of the University of Heidelberg, Germany, gave a presentation comparing different endovenous laser proceduplex ultrasoundres. He said there was no comparative clinical data with respect to different laser protocols available. Proebstle compared different kinds of laser wavelength and laser energy, looking at absorption in blood and water, vein wall perforation and vein wall shrinkages, treatment of related side effects and efficacy and duplex ultrasoundrability of occlusion.
He concluded that Linear Endovenous Energy Density (LEED) seems to be a reasonable parameter to exceed 100 joule/cm, and that Endovenous Fluence Equivalent may help to adjust low-energy electron diffraction LEED for classes of vain diameters. Proebstle also said 940 nm, 30 Watt continuous ELT improves results dramatically and that wavelength does not seem to be too important.
Lastly, but by no means least, Provensis, a subsidiary of BTG, has received approval from the FDA to resume clinical development of Varisolve, a novel microfoam treatment for varicose veins. Previously, the FDA suspended pre-clinical trials whilst the Agency investigated ‘hypothesized problems’ ie. do the micro-bubbles have any subclinical side effects? After a review the FDA accepted the company’s pre-clinical data and the company’s Phase II study protocol. Provensis is currently nearing completion of Phase III study in Europe.