Initial results of an ongoing first-in-man study in Colombia, that saw the implantation of a prosthetic venous valve in 15 patients, have demonstrated an improvement in clinical outcomes and quality of life. The promising findings were presented to delegates at the Southern Association for Vascular Surgery (SAVS) annual meeting (8–11 January 2020, Palm Beach, USA).
According to trial investigator Jorge H Ulloa (Universidad de los Andes, Bogota, Colombia), there was also a marked reduction in pain among “a complex and difficult-to-treat patient population”. In the USA, 2.4 million people are affected with chronic venous insufficiency, Ulloa et al noted in their abstract. Moreover, one million are treated for venous stasis ulcers, with few options available to patients who develop post-thrombotic disease secondary to deep venous reflux.
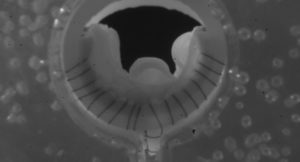
The new venous prosthetic valve, known as the VenoValve, is a combination of a stainless-steel frame and porcine aortic monocusp leaflet, and was developed to be surgically implanted into the deep venous system—the femoral popliteal vein—of patients with C5–C6 disease.
Endpoints of the study were to evaluate safety, “which is very important in a first-in-man study,” said Ulloa, who continued: “These include reflux by duplex ultrasound and femoral popliteal vein, as well as clinical assessment by a vascular surgeon. Also, pain scoring, the visual analogue scale (VAS) score and quality of life outcomes were evaluated by the patients during this study.”
In the trial, researchers included actual venous reflux greater than one second in C5 and C6 patients. “Superficial reflux was controlled or ablated prior to patients enrolling into this study,” Ulloa said. “All of [the patients] were able to walk by themselves and peripheral arterial disease (PAD) was ruled out by alternating blood flow (ABF).” Ulloa went on to explain that just three weeks prior to his presentation at the SAVS podium, the research team had completed its 11th case.
He drew attention to six patients who averaged at least six months of follow-up. “We have seen a 40% reduction in reflux, a 61% improvement in [the] Venous Clinical Severity Score (VCSS) or have significant clinical improvement, and all patients at six months have noted a significant reduction in their pain by the VAS score. Patient six increased the VAS and VCSS due to poor anticoagulation therapy and by lack of compliance.”
Ulloa added: “All cases have demonstrated a marked improvement in the reflux, with most of them reaching baseline except in patient six. Significant clinical improvements were also observed. Many patients went from moderate to severe to mild disease by clinical assessment.”
Summing up his findings, Ulloa concluded: “We had an overall improvement in reflux by 40%, a clinical improvement by 61% with an average of 8.4 points and a 57% pain improvement. The implantation technique has evolved a great deal since the first case was performed, with an average timing of 40 minutes. Our results of this feasibility study are on the way.
“We will evolve to a second phase, which will include a pivotal trial with more recruiting centres and increasing the number of cases to assess the performance of this prosthetic valve as an option for patients with C4B to C6 disease. Reflux quality calculations will be included in the next phase.”
In discussion of the study, Seshadri Raju (RANE Center, Jackson, Mississippi) praised the investigators, but zeroed in on what he identified as a flaw. “One criticism of the study is that clinical improvement data collection seems to have been rather rudimentary,” he said, addressing Ulloa.
“The technical improvement seems to be impressive enough, but needs to be connected to improvement in valve function. Reflux duration is a qualitative measure and cannot be used as a quantitative metric as done in this study, and as has been shown by numerous other authors not to be functional. The more appropriate measurement is reflux quality calculated from velocity duration and calibre.”






