A special session during the pre-conference Day of Innovation and Science at the American Venous Forum annual meeting (AVF; 20–23 February, Tucson, USA) presented the rare occasion for attendees to listen to and interact directly with the principal investigator of what has become one of the most talked about trials in the venous world in recent years—the ATTRACT trial.
Attendees were given the opportunity to hear in-depth analysis of the study from a variety of stakeholders and ask a number of questions with the goal of increasing the general understanding of the trial, including the protocol, the outcome measures and the results, as well as what it all means for current practice.
One of the key talks was that given by principal investigator Suresh Vedantham (Mallinckrodt Institute of Radiology, Washington University School of Medicine, St Louis, USA) who sought to clarify many of the misconceptions purported about the study, which, according to Vedantham may “not reflect a complete understanding of what is in the data”.
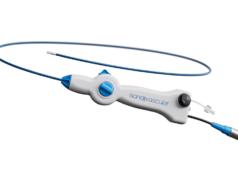
1.ATTRACT’s aim: Expanding the first-line use of pharmacomechanical catheter-directed thrombolysis (PCDT) in proximal DVT
ATTRACT was aimed at initially presenting deep vein thrombosis (DVT) patients; the purpose of the study was not to validate “salvage” PCDT, but to determine appropriateness of expanding PCDT to routine first-line use in proximal DVT. “No other study was as large and as broadly generalisable, as representative of the DVT clinical community in terms of its organisational leadership, as contemporary in selection of PCDT methods or as methodically sound, as there were a lot of precautions against bias,” Vedantham said.
2. The validity of the Villalta scale
There has been a lot of comment that the Villalta scale is invalid and unpublished. “I would push back on that. Yes, the initial abstract was not published, but at the time that we wrote the ATTRACT grant (2006), there had been 17 publications that described the reliability, validity, responsiveness and acceptability of the Villalta scale, and some of those reflect clear correlations with the anatomic-physiologic findings of venous disease on venography, ultrasonography and even direct measurement of ambulatory venous pressures. There are many more publications now. The idea that the Villalta scale does not measure venous disease, I find that hard to believe given all the information that I have seen,” he maintained.
3. Residual clot
Another misconception is the residual clot in ATTRACT trial patients or the idea that the “veins were not opened”. “Just to put this in perspective I went back to previous studies that had core lab review of the venograms after clot removal therapy—the CAVENT study and the National Venous Registry. I looked at their residual clot scores on the scales that were used, and found 9.3% residual clot in the CAVENT study, 9–40% residual clot in the National Venous Registry and 12.5% in the ATTRACT trial,” Vedantham said. He added that the clot removal efficacy in the ATTRACT trial was confirmed by both the operators (who visually assessed whether excellent flow was present in the iliofemoral and femoropopliteal vein segments on the venograms at procedure end) and independent reviewers at the core lab. The trial had better safety results (less bleeding) than previous studies with much less re-thrombosis, supporting the quality of the operators, and there was no difference in the PCDT effect in terms of whether it was done between zero to seven days or seven to 14 days.
As for the use of stenting and intravascular ultrasound (IVUS) and the idea that they were discouraged or not permitted, Vedantham said that the study protocol actually encouraged stenting in the iliac vein for lesions causing > 50% narrowing, robust collateral filling, or a mean pressure gradient more that 2 mmHg. “Really the way it was written was to encourage the use of iliac vein stenting, but a lot of the patients (43%) had femoropopliteal deep vein thrombosis which is not likely to be associated with an iliac vein lesion,” he clarified.
Similarly, IVUS, though it was not widely use in the trial, was not forbidden by the protocol, “but during the time the study enrolled, relatively few operators routinely used it for acute DVT patients… and if you are going to say that the study failed because IVUS was not used routinely, then you must also question the effectiveness of what we were doing between 1994 and 2014 (pre-IVUS),” he added.
4. The primary outcome
In terms of whether the trial would have been positive had the Venous Clinical Severity Score (VCSS) been used for the primary outcome, Vedantham maintained that this is not the case and the fourth common misconception associated with ATTRACT. “From the data,this trial would have been negative even if the VCSS ³4 had been used as the primary outcome and even if the iliofemoral DVT only had been studied,” he pointed out.
5. ATTRACT vs. CAVENT
A further misconception according to Vedantham is that the ATTRACT trial results are entirely inconsistent with those of the CAVENT trial. “Certainly there are differences, but in both studies, 40–50% of the lysed patients got post-thrombotic syndrome, so clearly we have big gaps that we need to fill. Further, if you count the number of patients with moderate to severe post-thrombotic syndrome using the Villalta scale in CAVENT versus ATTRACT, it was the exact same number: 6% absolute risk reduction,” he explained.
6. Trial findings vs. clinical observations
Vedantham stated that based on clinical observations, practitioners expected to see two main outcomes: first that post-thrombotic syndrome was going to be a lot more common in the iliofemoral group compared to the femoropopliteal group, and second that in the long run PCDT would reduce post-thrombotic syndrome occurrence and severity, improve quality of life and reduce venous thromboembolism over two years.
The first was true, “but only by a small margin of 50% in the iliofemoral group versus 44% in the femoropopliteal group. I think many of us would have expected more, and that is because we look in our clinical practices and in the published case series at a cherry-picked, referred group of patients that were the worst clotters, had the worst symptoms, but ATTRACT studied a different population altogether. So there is a difference between iliofemoral and femoropopliteal, but it may not be as large as we thought it would be.”
As for the second, “when it comes to the long-run, we have to consider what we really knew about the long-run in clinical practice,” Vedantham said, pointing out that in clinical practice, it is not common that DVT patients are followed as far out as two years by physicians that pay attention to post-thrombotic syndrome. “The study shows that even with iliofemoral DVT, we do not see all of them, we just see the ones that people send us. I think that gap between what this study showed about the long-term outcome and our clinical observations has a lot to do with the difference in those patient populations,” he added.
Way forward
As for the way forward and what the ATTRACT trial has accomplished despite its negative outcome, Vedantham hinted that once the secondary papers are published, the study will have clarified the proper role for the first-line use of PCDT in current practice. “I think the reduction of the unjustified PCDT use will reduce TPA complications, save lives and reduce disability, and the discordance of the findings on post-thrombotic syndrome occurrence versus post-thrombotic severity progression might be later viewed as a major, fundamental pathophysiological insight,” he concluded.