
Laser crossectomy of the GSV has been established as a more effective method of preventing secondary anterior accessory great saphenous vein (AAGSV) reflux than treatment modalities which leave stumps. As part of a randomised controlled study comparing the technique with infra-epigastric closure, it was also affirmed that consideration of AASGV anatomy is pivotal when making the right choice of strategy.
Results of the investigation were presented at International Union of Phlebology chapter meeting (UIP 2019; 25–27 August, Krakow, Poland) by Johann Chris Ragg (Berlin, Germany), who explained how his interest in this comparison of modalities developed. “Some years ago, I was shocked by a remark from a colleague, who said that occurrence of reflux of a previously healthy AAGSV after standard endovenous great saphenous vein (GSV) ablation may be higher than after surgical crossectomy. My own 8-year results had junction recurrence rates below 12% but were obtained with laser crossectomy. Due to this argument, we decided to find out what the difference is,” Ragg said.
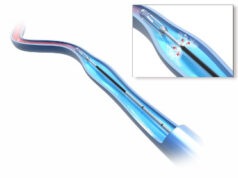
He continued: “When we started with venous lasers in 1999 as early pioneers, I had no other idea than to start GSV closure right from the femoral level, equivalent to surgical flush ligation, with total vein compression by precise coaxial perivenous local anesthesia (CPLA) manually injected with a 200mm G21 needle. Instead of a constant pullback rate, fibre pullback was done according to wall reaction in order to place as much energy as possible, but below wall disruption and below pain level (PAWR technique).”
According to Ragg, most later-on laser users preferred to ablate with a “safety distance” to the junction in order to prevent femoral EHIT (endovenous heat-induced thrombosis), and a less precise “tumescent anesthesia”. This method became a standard, as it was fast and easy to perform.
The aim of the randomized study was to compare infra-epigastric to femoral-level laser ablation, using identical device and techniques. 240 consecutive patients with GSV insufficiency (CEAP C2–C6; diameters 6.5–17.8 mm) were selected with the criteria of 1) reflux > 1,000 milliseconds from the saphenofemoral junction (SFJ, Valsalva test) 2) non-refluxive AAGSV and 3) no other refluxive branch of the SFJ undergoing endovenous laser ablation (EVLA; 1470nm, radial fibre, 50-80 J/cm) with CPLA. Participants were randomised to one of two groups: group A underwent laser crossectomy—defined as EVLA starting at the femoral vein level—while patients in group B were treated with EVLA starting below the epigastric vein junction. Follow-up including ultrasound was performed at day one, day 14 and after one, six, 12, and 24 months.
Presenting the results of the trial, Ragg commented: “Primary GSV occlusion was obtained in all cases, but with significant difference in the morphology. Using ablation from femoral level (group A), the outlet of AAGSV was covered in 118/120 cases (98.3%). At one-month follow-up, 102 of the 120 patients in this group showed no stump at all (85%). 18/120 (15%) had minor stumps of 5–17mm length, mean 11.5mm.
More than stump length, stump diameter was characteristic, measuring 18–29% of the previous native diameter in group A, in 17/18 cases (94.4%) presenting a run-off from the inferior epigastric vein. In group B, the entry to the AAGSV was covered in only 13 of 120 cases (10.8%). There were much larger GSV vein stumps present in all of the 120 patients, measuring 8–31mm in length, mean 23mm, and diameters of 55–87% of the native size). In both groups, there were no adverse effects and, in particular, no EHIT.
Within the two-year follow-up, AAGSV insufficiency was recorded in five of the patients (4.2%) after laser crossectomy (group A) and 26 of the patients (21.7%) in group B (p > 0.01). All refluxive cases were related to AAGSV with pre-treatment diameters of 5.5mm or more. Visible AAGSV varices were seen in 1/120 cases (0.8%, group A) versus 4/120 (3.3%, group B). Of these cases, none were symptomatic.
Ragg concluded: “If pressure stress or venous hypertonus at the SFJ is the problem, GSV closure will transfer pressure to the next large descending branch. Although it might take several years unto clinical manifestation, it makes sense to include the AAGSV entry in the ablation, in particular when AAGSV diameter is above 5.5mm. Standard ablation starting below the epigastric junction results in five-fold rates of later-on AAGSV reflux compared to laser crossectomy. That is the main result of this study.”
Furthermore, Ragg emphasised that “it is clear that laser crossectomy is superior to standard infra-epigastric ablation, but further ultrasound-based studies should follow, to clarify AAGSV vulnerability”.









Hi Johann,
It is interesting study, however why do you perform laser crossectomy instead of aagsv ablation?
The chance that 5.5mm trunk remains competent is low anyway. Have you tried using direct AAGSV Venaseal occlusion instead of laser ablation – it gives the same reSult but is simpler and faster.
Best regards