Medtronic has announced the initiation of its investigational device exemption (IDE) study for the Abre venous self-expanding stent system. The ABRE IDE Study will evaluate the safety and effectiveness of the Abre stent in patients with iliofemoral venous outflow obstruction.
The first procedure was performed in December of 2017, by Erin Murphy, director of the venous and lymphatic programme at Carolinas HealthCare System’s Sanger Heart & Vascular Institute in Charlotte, USA, and national principal investigator for the ABRE IDE Study in the USA.
The multicentre, single arm study intends to enrol 200 patients with deep venous disease from up to 35 sites throughout the USA and Europe. The primary efficacy endpoint will evaluate patency at 12 months, which is defined by freedom from occlusion and freedom from clinically-driven target lesion revascularisation (CD-TLR). The primary safety endpoint will evaluate the incidence of composite major adverse events (MAE) at 30 days following stenting of an obstruction in the iliofemoral venous segment. Data from the study will be used to support the Abre stent US pre-market approval (PMA) application for the treatment of symptomatic iliofemoral venous outflow obstruction in patients with venous occlusive disease.
“The launch of the ABRE IDE Study marks the beginning of an important journey to establish new options for the treatment of deep venous disease,” says Murphy. The first procedure was performed at Sanger Heart & Vascular Institute on a patient with Nonthrombotic Iliac Vein Lesion (NIVL) who is doing well post-treatment. We are excited to continue enrolment at our sites throughout the USA and Europe.”
Medtronic estimates deep venous obstruction affects more than 24 million individuals worldwide. Deep venous obstruction occurs when veins in the deep venous system become compressed and restrict blood flow. It can result in discomfort and pain, limit a patient’s mobility, and impair quality of life.
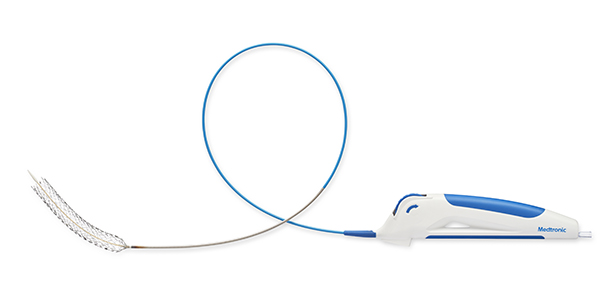
The Abre stent is an investigational device in the USA intended for permanent implant in the iliofemoral vein. It is pre-mounted on a 9 French delivery system and features a nitinol stent with a tri-axial shaft design. The stent utilises an open-cell design with three connection points between the cells that are intended to enable flexibility and conformability. Upon deployment, the Abre stent uses an optimised balance of strength and flexibility to exert an outward force and open the vein.
“Deep venous disease can cause pain, swelling, and blood clots, which can potentially be devastating to patients,” says Stephen Black, consultant vascular surgeon, Guy’s and St Thomas’ Hospital, London and European principal investigator for the ABRE IDE Study. “As a result, there is a critical need for treatment options that are safe, effective, and durable. We look forward to using the Abre stent in the restoration of patency in patients with deep venous disease.”
In the USA, Abre is an investigational device and not yet approved for commercial use. The stent received CE mark approval in April of 2017 and is intended for use in the iliofemoral veins for treatment of symptomatic venous outflow obstruction.









