Intravascular ultrasound (IVUS) imaging technology provides the current gold standard technique for detection and characterisation of venous disease, Erin Murphy writes. In this article, Murphy discusses the limitations of venography and outlines the use of IVUS for optimised outcomes in venous stenting.
Chronic venous obstructive disease can have a variable presentation that includes pain, heaviness, oedema, skin hyperpigmentation, lipodermatosclerosis, and eventually venous ulceration. While limb or loss of life in the chronic phase of disease is rare, quality of life measures can mirror that of other debilitating medical conditions, including congestive heart failure, chronic obstructive pulmonary disease, or diabetes.1,2
Venous stenting can relieve underlying iliofemoral and caval obstruction, and can result in dramatic improvement in the patient’s lower extremities and quality of life. These procedures have now become first-line surgical practice for venous obstruction. Reported long-term results are excellent.3
However, the durability of these procedures, are only obtainable with attention to detail during the procedure. Making use of your imaging is the most essential component of venous stenting. While venography has been a long-standing imaging technique, this technology has its limitations.
For the most part, venography is utilised to provide an overall initial gross assessment of vessel patency, collateralisation and flow. This allows you to develop an overall plan quickly. However, venography is not well suited to provide specific information—even with multiplaner venography, it remains inadequate. Instead, in venous disease, IVUS is your essential tool, and the gold standard for detection and characterisation of disease.
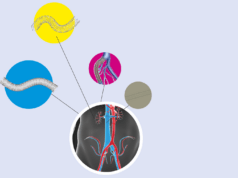
After crossing stenotic or occluded venous segments, IVUS is performed to guide the remainder of the procedure. The first role is to determine the degree of stenosis. The degree of stenosis can be determined by comparing the degree of stenosis to adjacent normal vein or to contralateral normal venous segments. However, stenosis in venous patients may be diffuse without adjacent normal segments of vein. In these cases, the degree of stenosis is determined by comparison with anatomic normals for each segment. The normal diameters of the common iliac vein, external iliac vein and the common femoral vein are 16, 14, and 12mm respectively, with expected areas of 200, 150, and 125mm2.
In comparison with IVUS, venography has proven to be a wholly ineffective means of determining degree of venous stenosis.
The Vidio trial was a multicentre, prospective trial in which multiplaner venography was performed and a treatment plan developed, followed by IVUS and a final treatment plan. IVUS detected 88% more lesions than venography and importantly, 29% of patients had a normal venogram despite IVUS revealing significant disease requiring stenting.4 In my series, venography missed 25% of lesions and underestimated disease in 69% compared to IVUS.5 Overall, venography has shown only around a 50% sensitivity.6
After identifying venous lesions and deciding to proceed with stenting, the next step is to identify your ideal stent size as well as stent landing zones. Sizing should be chosen so that the final stent selected is about 2mm larger than the reference vessel. This step is increasingly important as the effects of oversizing nitinol stents may be more dangerous than with the Wallstent (Boston Scientific), while undersizing can remain a problem which risks persistent obstruction or stent occlusion. Stents must then be landed in the healthiest available portion of the veins. This is an important measure to prevent early postoperative stent occlusion. Looking at the proximal landing zone first, the healthiest portion is most often the iliac confluence, but on venography, the confluence can be unclear and hard to identify. When it can be identified on venography however, the location of the confluence as compared to the location determined by IVUS can be off by as much as an entire vertebral body. Most commonly, IVUS determines the confluence to be higher than anticipated by venography. In these cases, if venography had been used, the stent could be landed too low, resulting in missed proximal lesions.5
Distally, stents are landed in the largest and least diseased segment above the profunda. However, improper distal landing zone is one of the most common reasons for early stent occlusion. When comparing venography to IVUS for determination of the best distal landing zone, venography can be off in up to 70% of cases, and IVUS often determines a higher landing zone.6 This places patients at risk of missed distal lesions, understenting and restenosis of the stent or reocclusion. Importantly, because of near universal recoil in the venous system, stent landing zones should be determined prior to balloon venoplasty.
After IVUS determination of the degree of stenosis and stent landing zones, the remainder of the procedure may proceed with venous balloon dilation and stenting. Pre-dilation is performed to break up the fibrous tissue prior to stenting. Large, noncompliant balloons are dilated to the size of intended stents. Stents are placed from inflow to outflow determined by pre-ballooning IVUS, and post-dilated.
IVUS is then again performed post to assure there are adequate areas and no shelving. Stagnant flow may also be visualised on IVUS, which may be secondary to unchangeable factors such as poor inflow, related to obstructive sheath placement in a small but dominant femoral vein, or could indicate a problem with the stent or outflow tract. Discovery of stagnant flow on IVUS should be an indication to recheck your outflow tract. If it is related to the inflow, however, recommendations can be made for anticoagulation, compression and mobility. Balloon venoplasty of inflow vessels may also be considered, and repeat venogram is performed to look for flow irregularities. The majority of collaterals are often resolved.
In conclusion, IVUS is an essential component of iliofemoral venous stenting procedures. Limitations of venography are not a limitation of the operator, but rather a limitation of the technology that cannot be overcome—even with experience. IVUS should be used during venous stenting procedures for the adequate initial assessment of degree and extent of disease, for the delineation of venous anatomy and determination of stent landing zones to guide stent placement, determination of stent sizing, and finally to detect early problems before leaving the operating room.
Erin Murphy is the director of the venous and lymphatic programme at Carolinas HealthCare System’s Sanger Heart & Vascular Institute in Charlotte, USA.
References
1 Lubberts B, Paulino Pereira NR, Kabrhel C, Kuter DJ, DiGiovanni CW. What is the effect of venous thromboembolism and related complications on patient reported health-related quality of life? A meta-analysis. Thromb Haemost. 2016 Aug 30;116(3):417-3.
2 Kahn SR, Shbaklo H, Lamping DL, Holcroft CA, Shrier I, Miron MJ, e al. Determinants of health-related quality of life during the 2 years following deep vein thrombosis. J Thromb Haemost. 2008 Jul;6(7):1105-12.
3 Razavi MK1, Jaff MR2, Miller LE2. Safety and Effectiveness of Stent Placement for Iliofemoral Outflow Obstruction: Systematic Review and Meta-Analysis. Circ Cardiovasc Interv. 2015 Oct;8(10).
4 Gagne PJ, Tahara RW, Fastabend CP, Dzieciuchowicz L, Marston W, Vedantham S, et al. Venography versus intravascular ultrasound for diagnosing and treating iliofemoral vein obstruction. J Vasc Surg Venous Lymphat Disord. 2017 Sep;5(5):678-687.
5 Murphy EH, Johns B, Alias M, Crim W, Raju S, Jayaraj A. Inadequacies of venographic assessment of anatomic variables in iliocaval disease. Abstract. J Vasc Surg. 2017 June;63(6)S:33S-34S.
6 Neglen P, Raju SR. Intravascular ultrasound examination of the obstructed vein. J Vasc Surg 2002. Apr;35(4):694-700.