Clinical outcomes with the Vici venous stent system (Boston Scientific) have been described as “very good”, according to a presentation of 24- and 36-month follow-up data at the Leipzig Interventional Course 2020 (LINC; 28–31 January, Leipzig, Germany). During his talk, first author Michael Lichtenberg (Klinikum Arnsberg, Arnsberg, Germany) added that while the findings are “promising”, longer-term follow up is necessary.
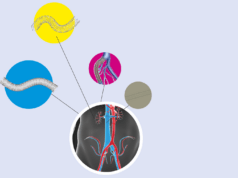
The close-cell Vici is a self-expanding, nitinol stent which, also accompanied by a delivery system for controlled stent placement, is available in a diameter of 12–16mm and a length of 60–120mm. Speaking on the key attributes of a venous stent, Lichtenberg stated: “The goal is to always have an ideal balance between strength, flexibility and lumen quality, though it has been found that the latter is one of the most important aspects in venous recanalisation.”
In order to test the efficacy and safety of Vici in a mixed cohort of patients with chronic venous outflow obstructions, Lichtenberg and colleagues conducted a retrospective study of patients who received the stent as early as 2013. Stent patency was evaluated by duplex ultrasound scanning, while clinical outcome was determined using the revised Venous Clinical Severity score (rVCSS).
In the 12-month data, 75 patients (49% female; median age 57 years; 82 limbs) with symptomatic significant venous outflow obstruction—who had stents placed in the iliofemoral veins—were followed up. Cumulative primary, assisted-primary, and secondary stent patency in the entire cohort at 12 months were 94%, 94% and 96%, respectively, while a clinical improvement (defined as a decrease of two or more rVCSS points) was observed in 81%, 81%, and 77% of patients at one month, six months, and 12 months, respectively.
Although there was no statistical difference in clinical outcome between subgroups of the cohort—those with nonthrombotic iliac vein lesions (NIVLs), and those with post-thrombotic obstruction (PTO)—the respective cumulative primary stent patency at 12 months was 100% and 87%.
In terms of adverse events, five limbs presented with stent occlusion: two of these limbs had no intervention, and another two remained patent after reintervention. In addition, four limbs had venous ulcers, three of which healed during the first 12 months of follow up.
“We always try to use a combination of angiogram and intravascular ultrasound (IVUS) together, to prove that we have achieved a very good lumen gain and aspect ratio (optimal close to one) in the stent implantation, and in my view this is an important process,” opined Lichtenberg, discussing technique.
Turning his attention to the 24- and 36-month data, Lichtenberg revealed that “there is nothing to report” with regard to the primary patency of the Vici venous stent. On the subject of clinical outcomes, he said: “Based on the patency rates, clinical outcomes remained very good. During follow up, the mean VCSS score improved significantly, immediately after the revascularisation. This also contributed to an improvement in CEAP classification.”
“These data are very much in line with the VIRTUS trial,” added the presenter. “This study showed a 12-month patency rate of 84%, meeting the primary endpoint of 72.1%. The 24-month data showed a patency rate close to 80%, which is quite similar to our data; the most common adverse event in both was target vessel revascularisation.”
Lichtenberg concluded: “We now have a lot of attractive venous stents on the market, and dedicated venous stents are certainly necessary. These clinical outcomes are very promising, though I think we should follow these patients for much longer, especially because long-term patency is quite different between peripheral arterial disease and venous disease. We are treating some very young patients, so long-term results are needed for 10 years, or possibly even longer.”