A single-centre experience using large, braided self-expanding stents for iliofemoral venous obstruction found “excellent” outcomes. Several useful techniques and pearls for improved outcomes are reported in the January edition of the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
Placement of large-diameter stents has become the mainstay treatment of symptomatic iliofemoral venous occlusion. However, factors affecting the clinical outcome and durable stent patency remain incompletely understood.
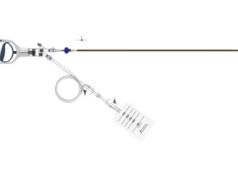
While the use of the large caliber, self-expanding stents in venous disease has been widespread, shortcomings such as less radial force at the ends and significant shortening remain issues in its deployment. As such, long-term assessment of its usage is now appropriate given first generation, dedicated venous stents are currently in clinical trial.
Researchers from The Vascular Experts in Darien, USA, led by vascular surgeon Paul Gagne, performed a retrospective review of their experience using self-expanding braided elgiloy stents to treat iliofemoral venous obstruction in 67 consecutive patients and 77 limbs treated in 2007–2014.
The patient demographic was characterised as:
- 55% male
- Median age 63 (range 47-83 years)
- 62% left-sided
- Having a median baseline Venous Clinical Severity Score (VCSS) score of 9 (3-23).
The deployed stents ranged in diameters of 10–22mm and in lengths of 40–90mm; of those, 82% were 14–18mm in diameter.
Additionally, 22% of stents were deployed into the common femoral vein while 8% involved the inferior vena cava (IVC), demonstrating the importance of landing in normal inflow and outflow vessels.
With regards to patency, at 72 months, those treated for non-thrombotic disease saw primary patency in 97%, as well as 100% primary assisted patency and 100% secondary patency.
Those treated for thrombotic disease, meanwhile, had a primary patency rate of 75%, as well as an 88% primary patency and 88% secondary patency.
At a median follow up of 26 months, 68% of patients showed a >4 point VCSS improvement, and no patient had experienced worsening symptoms.
Multivariate regression analysis revealed that only common femoral vein involvement predicted loss of primary patency (4.4 times more likely). Post-thrombotic lesions had loss of primary patency 6.9 times more likely, but this did not reach statistical significance (p=0.07).
The authors note that they changed their practice of stent sizing and protrusion into the IVC based on early failures in the series, and recommend under-sizing the stent relative to the IVC size. In addition, they limit protrusion of the proximal stent into the IVC. Since making these changes, the authors report no instances of contralateral deep vein thrombosis.
“Our experience found that stenting of chronic iliofemoral venous obstruction resulted in excellent long-term patency rates and significant clinical improvement for many patients,” noted notes Gagne. Although the stents present certain technical challenges, he said, “we have optimised our technique to work through these challenges to achieve good result.”
He further states that, “The analysis of most and least improved limbs found that improved outcomes were observed in patients who presented with more severe venous disease. The most improved subset was disproportionally composed of C6 patients with open ulcers, whereas one-third of the C3 patients treated in the overall series were among the least improved.”
Until randomised clinical trials confirm better efficacy for dedicated venous stents than conservative management, this important well documented series brings additional evidence to the long-term patency and clinical improvement afforded patients following use of large caliber, braided self-expanding stents for iliofemoral venous obstruction.