A new rotational thrombectomy device is safe and effective in the treatment of acute and subacute deep vein thrombosis in a single session of pharmacomechanical thrombolysis providing results of improved functional outcome.
The results of a multicentre registry with the new device were presented by Cüneyt Köksoy, Division of Vascular Surgery, Ankara University, Ankara, Turkey, at the European Society for Vascular Surgery (ESVS) Annual Meeting (18–21 September 2013, Budapest, Hungary).
“Deep vein thrombosis affects a significant proportion of the population. The treatment of deep vein thrombosis includes anticoagulation and compression stockings. However, a large number of patients with deep vein thrombosis develops post-thrombotic syndrome,” Köksoy said. “The open vein hypothesis is supported by studies that have linked poor thrombus clearance to venous valve dysfunction and recurrent thrombosis; studies that found an association between residual venous thrombus and post-thrombotic syndrome; and clinical trials that have suggested that systemic thrombolysis, surgical thrombectomy of catheter-directed thrombolysis reduces post-thrombotic syndrome.”
Köksoy told ESVS delegates that, in terms of early clot removal, each modality has its advantages and disadvantages. He added, “Pharmacomechanical thrombectomy refers to catheter-directed administration of a fibrinolytic drug directly into the venous thrombus with concomitant use of catheter-based devices to macerate the thrombus and speed thrombus removal. Pharmacomechanical thrombectomy can enable complete on-table removal of a thrombus in a single, one- to three-hour procedure, reducing the overall thrombolysis infusion time, dosage and length of stay.”
He said that there have been observational studies but no randomised trials in this area. “No single pharmacomechanical thrombectomy method is clearly superior to others. Catheter-directed thrombolysis with long lytic infusions is likely to be less efficient and less safe than pharmacomechanical thrombectomy and most endovascular surgeons or interventionalists prefer ‘faster’ pharmacomechanical methods that use lower doses of tPA and facilitate short stay in-patient deep vein thrombosis treatment. Until a randomised trial is conducted we need observational studies of new techniques and devices.”
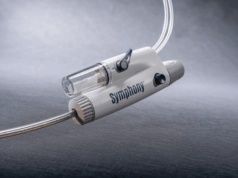
The aim of our study was to evaluate the safety and efficacy of pharmacomechanical thrombolysis utilising a new rotational thrombectomy device (Cleaner, Argon Medical Devices) for deep vein thrombosis in a nationwide four-centre registry.
The study enrolled patients with symptomatic deep vein thrombosis involving the femoropopliteal, iliofemoral and iliocaval segments, diagnosed by venous duplex. The procedure was performed under local anaesthesia, and all patients had an inferior vena cava filter placed. In some patients, catheter-directed thrombolysis or iliocaval stenting was performed after the procedure. Patients also received anticoagulation therapy and elastic stocking compression after the procedure.
Following diagnosis of acute or sub-acute lower extremity deep vein thrombosis, the device was inserted and pharmacomechanical thrombolysis was applied as “single-session” technique. At the end of the procedure patency was confirmed by contrast venography. The extent of lysis was graded from I to III. Grade III lysis was defined as complete resolution of thrombus on visual assessment of venograms. Grade II and I lysis were deemed present when the extent of thrombus resolution was 50–99% and <50%, respectively. The patients were evaluated for the efficacy and safety of thrombolysis and recurrent thrombosis at a mean follow-up of 3.5 (1.5–12) months.
Fifty three patients, 37 males and 16 females, mean age 54.3 years (17–84) underwent thrombolysis. The duration of symptoms was 19.8 days (3–92), and 22.6% patients had had symptoms for more than 30 days. Phlegmasia cerulea dolens was noted in six of the patients (11.3%). Mean amount of tPA was 20.7mg (10–50mg) and duration of procedure was 75.1 minutes (30–300).
There was one failure to advance the device. There was no device failures or adverse events associated with the device. Thirty two patients (60.4%) had complete thrombus (Grade III) resolution at the end of the procedure. Grade II and I lysis was noted in 19 patients (35.8%) and two patients (3.8%), respectively. “What is interesting is that there was an inverse relationship between the duration of symptoms and degree of lysis,” Köksoy said.
At follow-up, 83% of patients (44) had patent veins and two patients had patent iliac stents. Based on the Villalta score, mild to moderate post-thrombotic syndrome developed in 38% of patients. Long symptom duration at admission and occluded veins at follow-up were associated with post-thrombotic syndrome. Using rotational pharmacomechanical thrombolysis, successful lysis (more than 50%) was obtained in 96.2% of patients. This technique was not associated with clinically significant pulmonary embolism and major bleeding.
In conclusion, Köksoy said, “the technique has the potential to minimise morbidity and duration of hospital stay. Based on the present data, rotational pharmacomechanical thrombolysis warrants further investigation in large-scale studies.”