A new study suggests that the degree of intravascular ultrasound (IVUS)-determined iliofemoral venous stenosis does not appear to affect the initial clinical presentation, clinical-etiologic-anatomic-pathophysiological (CEAP) clinical class, supine foot venous pressure, clinical improvement, quality of life (QoL) improvement, stent patency, or reintervention rates after venous stenting. Arjun Jayaraj (The RANE Center for Venous and Lymphatic Diseases, Jackson, USA) and colleagues relay the findings of their recent investigation into the utility of the 50% stenosis criterion for patients undergoing stenting for chronic iliofemoral venous obstruction (CIVO) online in the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
The investigators detail that the criterion for venous stenting in symptomatic CIVO has been the “arbitrary” use of stenosis of ≥50% extrapolated from arterial literature. In order to assess the utility of this criterion, the research team evaluated the IVUS-determined degree of stenosis in a group of patients who had undergone stenting for QoL-impairing symptoms.
Jayaraj et al conducted a retrospective review of contemporaneously entered electronic medical record data from 480 continuous patients (480 limbs) with initial iliofemoral stents placed (2014 to 2017) for symptomatic CIVO impairing their QoL.
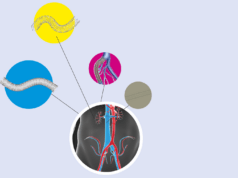
The IVUS-determined normal minimal luminal areas for the common femoral vein (125mm), external iliac vein (150mm), and common iliac vein (200mm) were used to group limbs as having <50% (low-grade stenosis [LGS]) or ≥50% (high-grade stenosis [HGS]) stenosis, Jayaraj and colleagues communicate in their paper. They specify that, of the 480 limbs, 283 and 197 were in the LGS and HGS groups, respectively, also noting a preponderance of women, left laterality, and post-thrombotic syndrome in both groups.
The authors report that, at baseline, although no difference was found in the visual analogue scale (VAS) pain score between groups, the LGS group had a higher venous clinical severity score (VCSS) than did the HGS group (p=0.05). In addition, they convey that the baseline median supine foot venous pressure was 15 and 14mmHg in the LGS and HGS groups, respectively (p=0.17).
At 24 months after stenting, Jayaraj et al reveal that the mean VCSS had improved from 6.3 to 4.4 (p<0.0001) and from 5.7 to 3.7 (p<0.0001) in the LGS and HGS groups, respectively, without significant differences between the two groups (p=0.07). In addition, they found a greater prevalence of ulcers in the LGS group (18% vs. 11%; p=0.04), with no difference in healing (p=0.41) or recurrence rates (p=0.36).
The QoL scores had improved in both groups (LGS, from 58 to 37 [p<0.0001], the authors continue; HGS, from 61 to 35 [p<0.0001]), without differences between the two groups (p>3), adding also that no significant differences in stent patency or reintervention rates were found. Finally, they note that a baseline composite chronic venous insufficiency score (CCVIS)—incorporating the VAS score, VCSS, and chronic lower limb venous insufficiency questionnaire-20 items (CIVIQ-20)—of ≥84.5, ≥86.9, or ≥105.3 was needed for a 30-, 40-, or 50-point improvement in most limbs after stenting.
“We need to move away from the ‘stenting for the degree of stenosis concept’ to stenting for symptoms impairing the patient’s QoL,” the authors write in their discussion. They stress that the goal for the treatment of patients with CIVO is to improve their QoL and not typically to save their limb and/or life, which they add are important considerations in the treatment of peripheral arterial disease (PAD).