A new review concludes that the implementation of clinical guidelines for the management of patients with deep vein thrombosis (DVT) varies among countries, from strict adherence to no adherence at all. “In this content,” suggest authors Carla Rognoni (SDA Bocconi School of Management, Milan, Italy) and colleagues, “the use of registries may be a useful tool to investigate the clinical practices and to produce findings that may be generalisable across populations.”
A new review concludes that the implementation of clinical guidelines for the management of patients with deep vein thrombosis (DVT) varies among countries, from strict adherence to no adherence at all. “In this content,” suggest authors Carla Rognoni (SDA Bocconi School of Management, Milan, Italy) and colleagues, “the use of registries may be a useful tool to investigate the clinical practices and to produce findings that may be generalisable across populations.”
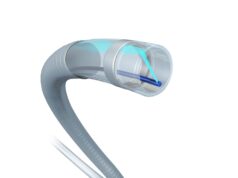
Writing in the Journal of Vascular Surgery: Venous and Lymphatic Disorders, the authors stress that DVT is “one of the major health problems worldwide”, noting its association with potentially serious outcomes related to mortality and morbidity. Against this background, the research team aimed to give a current view on how DVT patients are managed in routine practice compared to recommendations of published clinical guidelines.
Rognoni et al conducted a literature review on studies reporting diagnostic and treatment patterns for acute DVT. They evaluated four dimensions to compare differences between clinical practice and clinical guidelines recommendations: diagnostic pathway, prescription of pharmacological treatment and related duration, and prescription of compression therapy. For each aspect, the authors detail that the agreement with the corresponding guideline has been estimated as a percentage ranging from 0% (no agreement) to 100% (full agreement).
The team found that a total of 16 studies reported clinical practices in 10 countries. They report the following key findings:
- Japan showed the highest agreement with guidelines, followed by the UK and Switzerland
- Hong Kong showed the highest agreement with diagnosis guidelines, Spain for drug treatment, UK for treatment duration, and France for compression therapy
- Conversely, Germany reported a complete disagreement with guidelines for diagnosis, followed by low agreement level by the UK and Italy, while Switzerland reported the lower agreement level with prescription of compression therapy
Based on these outcomes, Rognoni and colleagues conclude that registries managed at national level may help to provider real-world data on the management of DVT patients. They elaborate: “Registries should enrol consecutive patients fulfilling specific criteria, possibly with no limits on time duration. Moreover, patients generally excluded from interventional clinical trials, like patients affected by renal insufficiency or at risk for major bleedings, pregnant, or elderly patients, should be included in registries so that findings may be generalisable across populations.”