Twelve-month results from the SENTRY trial evaluating the Sentry bioconvertible inferior vena cava (IVC) filter (Novate) have shown a 0% rate of symptomatic pulmonary embolism, no instances of device failure and a 96% rate of bioconversion. Presenting that data at the Vascular Interventional Advances 2017 conference (VIVA; 11–14 September, Las Vegas, USA), principal investigator Michael Dake (Stanford, USA) said that the data represent “an important paradigm shift in the prevention of pulmonary embolism”.
IVC filters are a controversial technology. Between 2005 and 2010, the introduction of retrievable filters led to their increased use. However, a high incidence of complications associated with IVC filters led to a US Food and Drug Administration (FDA) advisory and a decline in their use.
Pulmonary embolism, on the other hand, “is not controversial,” Dake said, with an incidence of 400,000–600,000 each year in the USA alone, accounting for 50,000–200,000 fatalities. One in every 10 hospital deaths is pulmonary embolism-related, and each event costs approximately US$52,000 to treat. “Used correctly, IVC filters save lives and reduce injury and cost related to pulmonary embolism, while survival benefit has been shown in appropriate populations,” Dake argued. However, he continued, “Existing retrievable technology has not met the needs of patients and healthcare systems.”
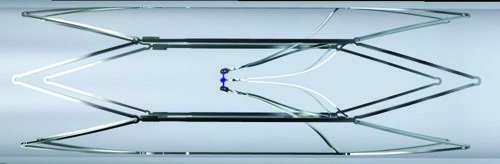
The Sentry IVC filter—which received FDA 510(k) clearance in February 2017—consists of a stable frame with filter arms held together by a bioabsorbable filament. This provides protection against pulmonary embolism during the transient risk period, before bioconverting via hydrolysis and releasing the arms which then retract to the IVC wall, leaving a patent lumen. This reduces the risk of IVC occlusion and removes the dangers and costs associated with filter retrieval. The FDA has published two warning letters recommending the retrieval of IVC filters after the transient risk period for pulmonary embolism subsides, which is typically beyond 30 days.
The SENTRY trial enrolled 129 patients requiring pulmonary embolism protection across 23 sites. Of those enrolled, 67.5% had current pulmonary embolism and/or deep vein thrombosis at the time of enrolment. All patients had contraindication to anticoagulation for all or some of the protection period. The primary factor for filter placement was surgery (n=77, 59.7%), followed by medical condition (n=28, 21.7%) and trauma (n=8, 6.2%).
The trial is “one of the most imaging-intensive studies conducted to date” analysing IVC filters, Dake noted, using ultrasound and venogram for the index procedure, ultrasound and computed tomography venography at one month, X-ray at two months, computed tomography at six months, X-ray at 12 months and computed tomography venogram at 24 months.
Dake reported 100% technical success and 100% freedom from symptomatic pulmonary embolism out to 60 days. There were two (1.8%) symptomatic caval thromboses which were treated and did not reoccur. There was no device tilting, migration, embolisation, fracture or perforation. At 12 months, no new symptomatic pulmonary embolisms were reported and there were no device-related complications. No secondary filters were placed to extend the pulmonary embolism protection period beyond 60 days.
The bioconversion rate of the filter filament was 96%, which “compares favourably” with published retrieval rates, Dake said. In the 18 patients who had a clot identified in the filter via one-month computed tomography venography, there were no symptomatic pulmonary embolisms. No IVC stenoses were reported at 12 months.
“This study offers us a new design and a new perspective on IVC filtration,” Dake concluded. Two-year follow-up is currently in progress.












