Nicolas J Mouawad (McLaren Health System, Bay City, USA) urges vascular surgeons to “get out of their comfort zone” and become more involved in pulmonary embolism (PE) care.
With over one million cases of deep vein thrombosis (DVT) and/or PE diagnosed each year in the USA alone,1 the management of patients with venous thromboembolic disease (VTE) is a critical public health concern.2 So much so that in 2008, the US Surgeon General declared a formal call to action against VTE. Despite an initial modest increase in awareness, it has been the recent COVID-19 pandemic that truly erupted a flurry of VTE therapies and catapulted this pathology from the sidelines to center-stage. Although DVT and PE are a continuum of the same disease state, untreated acute PE has a mortality of 30%.3 The severity of impact is primarily based on the embolic burden and the resultant effect on the right ventricle (RV), in addition to underlying comorbid conditions. The vicious cycle commences with acute increases in pulmonary arterial pressure secondary to the embolic obstruction which increases right ventricular afterload, increasing RV myocardial oxygen consumption and impairing RV contractility. This in turn subsequently affects the left side manifest by decreased cardiac output that can eventually lead to cardiogenic shock and death.
Pulmonary embolism response teams (PERTs) have emerged as an effort to battle the crisis of pulmonary emboli. Akin to “doctor-heart” for ST-elevation myocardial infarctions (STEMIs) and code stroke activations, the PERT is a multidisciplinary team focused on early triage, assessment, risk stratification and rapid coordination of an organised response to mobilise resources as necessary for PE care. These traditionally have been composed of interventional medical specialties with surgical counterparts as backup. The role of the vascular surgeon in the management of PEs varies widely and is based on their interest, their comfort (particularly navigating the heart), geography and the institutional politics.
The main issue in my opinion is that it feels outside of our “comfort zone” to be in the thorax. Whether surgically or by endovascular means, the thorax has historically been a black box—a void—for the vascular surgeon. From an interventional perspective, it is a domain of cardiothoracic surgery, interventional cardiology and interventional radiology, among some others. Furthermore, dedicated training paradigms have not been established for formal education in navigating the heart and the pulmonary vasculature for vascular surgeons. Most of us that are involved in PE care learned it from our interventional colleagues, training courses, or “on the job”. But why do we not take a more active role in this disease process? After all, we are vascular specialists very comfortable in diseases of the arteries, veins and lymphatics, whether medical, minimally invasive or maximally open.
And who gets an intervention? Unfortunately, risk stratification of patients with PE remains in development. The most common system separates them into low risk, intermediate risk, and high risk. An in-depth evaluation of cost, resource utilisation, risk and safety profiles as well as clinical efficacy, such as Hi-Peitho, Peerless 2, STORM-PE, PE-TRACTS, among others, are currently underway to help answer many of these questions.
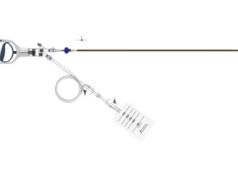
For those that qualify for intervention based on currently used criteria, vascular access is obtained in the standard fashion with ultrasound guidance. Caval venography is performed to ensure no anatomic abnormality, thrombosis or clot in transit. The right heart is then catheterised—I am a fan of the angled pigtail more so than a balloon-tipped catheter such as the Swan-Ganz as I feel its shape mirrors the anticipated trajectory. For each one of my PE interventions, a full right heart catheterisation is performed. A comfort with waveform analysis traversing right atrium, right ventricle and into the main pulmonary artery is paramount. These are standard displays in a cardiac catheterisation laboratory although not usual in the operating suite, so depending on your site of care, it is important to equip your lab with the ability to transmit and display these data. Clearly it will help monitor critical patient vitals and also assist in evaluating the effectiveness of some interventions. The procedure is then completed in the standard fashion.
Just as we have adopted many new disruptive technologies for the management of our patients, the pulmonary vasculature is an extension of the vascular tree we are trained to treat. I submit that it is time we branch out in the pulmonary arterial tree and become comfortable navigating the heart. We are trained for quick decision making in high-stakes situations. It is time to dust off our old physiology textbooks and revisit right heart pressures, pulmonary vascular resistance and dynes/sec! A multidisciplinary group is imperative for the management of patients with PE—and for a successful PERT—and vascular surgeons should get out of their comfort zone and play an active role in this patient population and pathology. We have a duty to our trainees to develop training paradigms to tackle all components of vascular disease and offer a familiarity and applicability of endovascular concepts while addressing barriers to implementation. Through continued awareness, education, and support, we can help cement vascular surgery as an integral component of comprehensive PE care and focus on improving PE patient outcomes.
Nicolas J Mouawad is chief and medical director of vascular and endovascular surgery at McLaren Health System in Bay City, USA.
References
- Lutsey PL, Zakai NA. Epidemiology and prevention of venous thromboembolism. Nat
Rev Cardiol. 2023 Apr;20(4):248–262. doi: 10.1038/s41569-022-00787-6. Epub 2022 Oct 18. PMID: 36258120; PMCID: PMC9579604. - US Department of Health and Human Services. Surgeon General’s call to action to prevent deep vein thrombosis and pulmonary embolism 2008. http://www.surgeongeneral.gov/topics/deepvein.
- Bĕlohlávek J, Dytrych V, Linhart A. Pulmonary embolism, part I: epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and non-thrombotic pulmonary embolism. Exp Clin Cardiol. 2013 Spring;18(2):129–38. PMID: 23940438; PMCID: PMC3718593.