A retrospective review, presented as a late-breaking clinical trial at The VEINS (Venous Endovascular Interventional Strategies) 2022 (30–31 October, Las Vegas, USA), indicates that single-session thrombectomy for the treatment of iliofemoral deep vein thrombosis (DVT) is associated with reduced intensive care unit (ICU) cost when compared with thrombolysis.
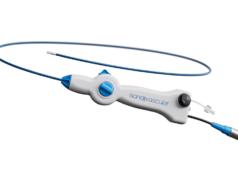
Presenter John Filtes (Columbia University Irving Medical Center, New York, USA) noted that lower extremity DVT is a major cause of morbidity in the USA, with significant associated healthcare costs. For iliofemoral DVT, he said, catheter-directed therapies lead to reduction in venous hypertension and inflammatory response to the acute thrombus, thereby reducing clinically significant chronic venous insufficiency, or post-thrombotic syndrome.
While two-session catheter-directed thrombolysis often requires an overnight ICU stay to monitor for bleeding and a second procedure for stenting, the presenter stated, mechanical thrombectomy devices have recently been developed that remove the thrombus using a combination of suction techniques—without the need for thrombolytics—and allow for stenting in a single session.
In Filtes and colleagues’ retrospective review of all patients who underwent thrombectomy and thrombolysis for the treatment of iliofemoral DVT at two large medical centres in the 10-year period from 2011 to 2021, the research team sought to compare costs of postprocedural intensive care for patients treated with single-session mechanical thrombectomy versus thrombolysis for DVT (often double-session).
Filtes reported at The VEINS 2022 that thrombolysis was associated with approximately US$6,000 of additional intensive care costs compared with single-session thrombectomy. Additionally, he revealed that thrombolysis incurred the additional cost of thrombolytics, which were not used for thrombectomy.
The presenter addressed some limitations of the study, including its retrospective nature, which he said “prevents controlling for extraneous factors potentially affecting outcomes”. In addition, he mentioned that patient selection for thrombectomy or thrombolysis was not uniform across providers or institutions.
Closing his presentation, Filtes presenter stressed that future studies should aim to analyse healthcare cost associated with treatment of DVT, inclusive of ICU costs, procedure costs, and physician costs.