While various treatment regimens for the “unique complication” of endothermal heat-induced thrombosis (EHIT) following endovenous ablation have been developed, Lowell S Kabnick tells Venous News, none have achieved universal acceptance. That is, he argues, until now. In this article, Kabnick details the history and development of EHIT treatment and classification, culminating in the recent publication of the joint American Venous Forum (AVF) and Society for Vascular Surgery (SVS) EHIT guidelines.
Early adopters of endovenous thermal ablation noticed that there was a unique complication that sometimes occurred—thrombus extension into the deep system, later known as EHIT. In 2002, we reported 286 limbs with a 1% incidence of EHIT.1 In 2003, Robert Kistner (Kistner Vein Clinic, Honolulu, USA), Robert Merchant (Reno Vein Clinic, Reno, USA), and I compiled our data and reported on 1,150 ablated veins with a 0.4% rate of EHIT.2 Alarmingly, at the 2004 AVF, Enrico Ascher (New York University Langone Medical Center, New York, USA) and Anil Hingorani (Vascular Institute of New York, New York, USA) cautioned all of us by reporting their early thermal experience with a 16% incidence of EHIT.3
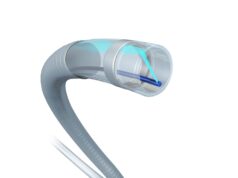
After analysing many cases of EHIT from three different institutions, it became clear that there were different patterns of thrombus extension. In 2006, I presented the definition and classification of EHIT at the AVF. The Kabnick EHIT classification is defined as follows: EHIT 1, venous thrombosis to the superficial/deep junction and not extending into the deep system; EHIT 2, venous thrombosis into the deep venous system, non-occlusive, with a cross sectional diameter of less than 50%; EHIT 3, venous thrombosis into the deep system, non-occlusive thrombus, with a cross sectional diameter of greater than 50%; and EHIT 4, total occlusion of the deep vein.
Various treatment regimens have been developed and modified without universal acceptance. With this in mind, the AVF recognised the need to develop practice EHIT guidelines that could be adopted universally. A writing group was organised and charged with establishing the EHIT definition, discussing the available EHIT classification systems, evaluating risk factors and prevention strategies, and appraising treatment options. We utilised four scientific repositories to identify potential publications related to EHIT: Pubmed, Embase, Corchrane, and Web of Sciences. Our writing group identified two EHIT classification systems, Kabnick and Lawrence, and noticed that the descriptors were similar.
After much deliberation, the AVF developed their classification system, which is essentially a minor revision to the Kabnick classification with regards to only EHIT 1—thrombus without propagation into the deep vein. Added to EHIT 1 was the following: a) thrombus peripheral to the superficial epigastric vein and b) thrombus central to the epigastric vein, up to and including the deep vein junction.
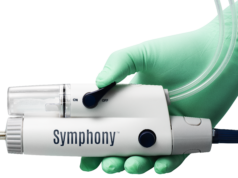
There are 15 guidelines regarding EHIT, which are published in the Journal of Vascular Surgery: Venous and Lymphatic Disorders and Phlebology.4 I have included the treatment guidelines regarding EHIT (Figure 1).
For further information, please refer to the entire article, ‘Classification and treatment of endothermal heat-induced thrombosis: Recommendations from the American Venous Forum and Society for Vascular Surgery’, co published in the Journal of Vascular Surgery and Phlebology.4
References
- Merchant RF, DePalma RG, Kabnick LS. Endovascular obliteration of saphenous reflux: A multicenter study. J Vasc Surg 2002 Jun;35(6):1190–6.
- Merchant R Jr, Kistner RL, Kabnick LS. Is there an increased risk for DVT with the VNUS closure procedure? J Vasc Surg 2003 Sep;38(3):628.
- Hingorani AP, Ascher E, Markevich N, et al. Deep venous thrombosis after radiofrequency ablation of greater saphenous vein: A word of caution. J Vasc Surg 2004 Sep;40(3):500–
- Kabnick LS, Sadek M, Bjarnason H, et al. Classification and treatment of endothermal heat-induced thrombosis: Recommendations from the American Venous Forum and Society for Vascular Surgery, co published in Journal of Vascular Surgery and the Journal of Phlebology. J Vasc Surg Venous Lymphat Disorder and Phlebology 2020. In press.
Lowell S Kabnick is a venous specialist at Kabnick Vein Center in Morristown, USA.
Figure 1. EHIT treatment guidelines
“Guideline 1.5: American Venous Forum EHIT classification system. We suggest preferential use of the unified American Venous Forum EHIT classification system to standardize ongoing reporting, given that it maintains the essence of the Kabnick and Lawrence classification systems, remains recognizable, and may be used for ongoing meta-analyses and systematic reviews. It is a four-tiered classification: I, junction; II, >50% lumen; IV, occlusive deep venous thrombosis. [BEST PRACTICE]
Guideline 3.1: Classification system. We suggest the stratification of treatment based on an accepted EHIT classification system. [BEST PRACTICE]
Guideline 3.2: Treatment for EHIT I. We suggest no treatment or surveillance for EHIT I. [GRADE – 2; LEVEL OF EVIDENCE – C]
Guideline 3.3: Treatment for EHIT II. We suggest no treatment of EHIT II but do suggest weekly surveillance until thrombus resolution. In high-risk patients, consideration may be given to antiplatelet therapy vs prophylactic or therapeutic anticoagulation with weekly surveillance. Treatment would cease after thrombus retraction or resolution to the saphenofemoral (GSV) or saphenopopliteal (SSV) junction. [GRADE – 2; LEVEL OF EVIDENCE – C] (Figure 2)

Guideline 3.4: Treatment for EHIT III. We suggest treatment with therapeutic anticoagulation for EHIT III, weekly surveillance, and cessation of treatment after thrombus retraction or resolution to the saphenofemoral (GSV) or saphenopopliteal (SSV) junction. [GRADE – 1; LEVEL OF EVIDENCE – B]
Guideline 3.5: Treatment for EHIT IV. We suggest that treatment should be individualized, taking into account the risks and benefits to the patient. Reference may be made to the Chest guidelines for the treatment of deep venous thrombosis. [GRADE – 1; LEVEL OF EVIDENCE – A]
Guideline 4.1: Management of EHIT for the SSV. We suggest that management and treatment for EHIT as it relates to the SSV parallel those for the GSV. [GRADE – 2; LEVEL OF EVIDENCE – C].”4