Anna Louise Pouncey revealed at the European Venous Forum annual meeting (EVF; 28–30 June, Athens, Greece) the findings of the GSTT venous team (Guy’s and St Thomas’ NHS Foundation Trust & Kings College London, London, UK) that early use of adjuvant AngioJet thrombectomy (Boston Scientific) resulted in reduction in post-thrombotic syndrome, equivalent vessel patency, and a reduction in the overall dose and duration of lysis.
Deep vein thrombosis (DVT) causes over 24,000 deaths a year in the UK, costing around £1 billion. For patients who have an iliofemoral DVT, the risk of developing post-thrombotic syndrome is 50%, and can result in severe consequences. In light of this, the American Venous Forum recommends that physicians should attempt early clot removal with lytic techniques. Percutaneous catheter-directed thrombolysis is often used to treat acute iliofemoral DVT, but the efficacy of this treatment and adjunctive pharmacomechanical modalities is not yet determined.
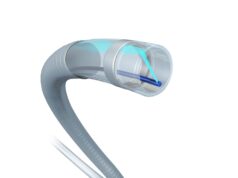
Whilst catheter-directed thrombolysis uses a multiple side-holed catheter to infuse lytic agents into the clot directly, working to soften and break it down, AngioJet rheolytic thrombectomy uses pressurised saline jets, to macerate the thrombus and aspirate material back into the catheter. The AngioJet has an additional mode—the “powerpulse” mode; involving active spraying of lytic agent into the clot, allowing time for it to soften, and, “leading to more success when using the rheolytic mode”, Pouncey noted.
Pouncey and the GSTT venous team aimed to retrospectively compare the outcome of patients who had been treated with catheter-directed thrombolysis alone, to those treated with the addition of AngioJet pharmacomechanical thrombectomy. They performed a single-centre retrospective cohort study, selecting all patients with symptomatic acute iliofemoral DVT treated between 2011 and 2017. A total of 151 cases were identified, consisting of 81 patients treated with catheter-directed thrombolysis and 70 with adjuvant use of AngioJet thrombectomy. Patient demographics, duration of symptoms, thrombosis risk factors and modality of treatment were collected. Four outcome measures were chosen: the incidence of post-thrombotic syndrome (measured by Villalta scores), primary, primary-assisted and secondary patency, lytic time and dose and the incidence of complications.
Baseline demographic data and prevalence of risk factors were comparable between groups. Incidence of post- thrombotic syndrome, measured by Villalta score at six months and one year, were equivalent (p=0.028). The analysis of cases treated with catheter-directed thrombolysis versus AngioJet showed no significant difference in primary, primary-assisted and secondary patency over two years. Addition of AngioJet thrombectomy resulted in a reduction in lysis duration of 40 hours (95%, CI:34–46) versus 53 hours (95%, CI:49–58, p=0.0001) and a reduction in lytic dose: 49mg (95%, CI:42–55) compared with 57mg (95%, CI:52–61) for catheter-directed thrombolysis. This reduction was accentuated in cases initially treated with “powerpulse” AngioJet thrombectomy: 27 hours (95%, CI:20–34) and 42mg (95%, CI:34–50).
Incidence of complications were found to be comparable between groups, with a major bleed rate of 0.66%—a rate in line with the current literature. The incidence of haemaglobinuria was increased following AngioJet thrombectomy (18.6% vs. 3.7%), but, no statistically significant difference in acute kidney injury was observed (4.3% vs. 1.2%, p=0.244). A slight increase in minor bleeding occurred in the catheter-directed thrombolysis group, which could be attributed to longer lytic times. One fatality—due to a haemorrhagic stroke—occurred in the catheter-directed thrombolysis group. This occurred three hours into lysis, due to an undiagnosed arteriovenous fistula. Overall, the authors felt there was an adequate safety profile for both treatment modalities.
Results from both catheter-directed thrombolysis and AngioJet cohorts had excellent Villalta scores and a low level of post-thrombotic syndrome. Both treatment modalities resulted in equivalent vessel patency. Importantly, the study found that AngioJet reduces lysis dose and duration, which is potentially cost-effective and safer for the patient. This improvement was accentuated in patients commenced on “powerpulse” mode, which reduced lysis time to just under 27 hours.
In relation to future implications, the GSTT venous team are currently conducting a health economic analysis, with a view to optimising the acute DVT pathway. With increasing pressures on the current health system, reducing patient transit time would be of great economic advantage, all-the-while providing as many as possible with improved symptomatic relief. The GSTT venous team attribute their low rate of post-thrombotic syndrome to attention to detail at every step of the patient journey. This includes judicious patient selection, early treatment, attention to anticoagulation, stenting healthy-to-healthy, and rigorous post-operative surveillance. Pouncey stated: “This is a moving field that is improving… attention to detail and discussion about the topic is important in terms of making sure we can all provide a better service.”