Compression stockings might be unnecessary to prevent blood clots in most patients undergoing non-emergency (elective) surgery, finds a clinical trial published by The BMJ today.
Compression stockings might be unnecessary to prevent blood clots in most patients undergoing non-emergency (elective) surgery, finds a clinical trial published by The BMJ today.
The results of the Graduated compression stockings as adjuvant to pharmaco-thromboprophylaxis in elective surgical patients (GAPS) randomised controlled trial suggest that giving anti-clotting drugs alone is just as effective and, as such, the researchers say current guidelines based on historical data should be revised.
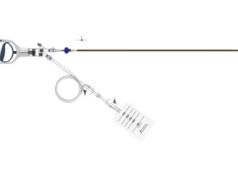
Current guidelines recommend using a combination of graduated compression stockings and anti-clotting drugs for patients undergoing elective surgery who are at moderate or high risk of venous thromboembolism (VTE).
However, in recent years, rates of VTE after surgery have fallen significantly due to improved care and drug therapy, leading some doctors to suggest that this combination might no longer be necessary.
Consequently, a team of UK researchers set out to investigate whether the use of graduated compression stockings offers any additional benefit to anti-clotting drugs to prevent VTE in patients undergoing elective surgery.
Their findings are based on 1,858 adult patients at moderate or high risk of VTE who underwent non-emergency surgery at seven NHS hospitals across the UK between May 2016 and January 2019.
Patients were randomly split into two groups. A total of 937 patients were only given anti-clotting drugs (low-molecular-weight heparin or LMWH) during their hospital stay and were asked not to wear any kind of compression stocking for 90 days after surgery. The remaining 921 patients were given the same anti-clotting drugs and were asked to wear graduated compression stockings during their hospital stay.
The main outcome was a scan showing deep vein thrombosis or pulmonary embolism within 90 days of surgery. Other measures included quality of life, adverse reactions to anti-clotting drugs, and death from any cause.
The researchers found that VTE occurred in 16 out of 937 (1.7%) patients in the drugs only group compared with 13 out of 921 (1.4%) patients in the drugs plus stockings group.
Both deep vein thrombosis and pulmonary embolism occurred in 2 out of 937 (0.2%) patients in the drugs only group compared with 1 out of 921 (0.1%) in the drugs plus stockings group.
Little or no differences between groups were found for other measures including quality of life up to 90 days after surgery, adverse drug reactions or deaths.
The researchers point to some limitations, such as the possibility of missed scans, but say this would probably not have influenced the overall findings. Results were also similar after further analyses, suggesting that the findings withstand scrutiny. As such, they say that in patients who have elective surgical procedures and are at moderate or high risk of venous thromboembolism, preventive drug treatment alone is “non-inferior” to a combination of drug treatment and graduated compression stockings.
Lead author Joseph Shalhoub and senior author Alun H Davies (both Imperial College Healthcare NHS Trust, London, UK) spoke to Venous News about the results of the GAPS trial. They commented on the significance of the study: “VTE following surgery is a major concern and this has rightly lead to the development of numerous guidelines. The use of mechanical thromboprophylaxis, particularly graduated compression stockings, are a prominent feature amongst many guideline recommendations. Recently, questions have been raised in relation to the benefit of GCS [graduated compression stockings], particularly when used in combination with pharmacological thromboprophylaxis.”
Commenting on how the trial may influence practice, they suggested that “the trial should prompt the review of guidelines around prevention of hospital acquired thrombosis”.
They continued: “We feel that, based on the trial results, GCS are no longer indicated in this surgical patient group. The impact for these patients is that they will no longer need to wear GCS, which many find uncomfortable and have been associated with complications.”
Considering the implication for health systems, Shalhoub and Davies remarked that “cost savings in relation to providing and applying GCS to medium and high VTE risk elective surgical patients have been estimated as being more than £63 million per year in England alone; funding and resources which may be re-allocated for patient benefit.”
Finally, they commented that “the trial indicates the role of GCS for thromboprophylaxis in other patient groups should also be looked at.”
Cliff Shearman (University of Southampton and University Hospital Southampton Foundation Trust, Southampton, UK), vice president of the Royal College of Surgeons (RCS) commented on the results of the trial: “We welcome this well-designed trial, which suggests that there is no need to wear compression stockings in hospital following surgery to prevent VTE. Patients find stockings inconvenient and fitting them takes up valuable nurse time. This study suggests we can save the NHS money and also save staff time by making a simple change, that improves perioperative practice.”