The pursuit of a cure for deep venous valvular reflux—long considered to be the “holy grail” of deep venous disease—is underway, with new technologies set to address a longstanding unmet clinical need across the globe.
Chronic venous disease affects nearly 25 million in the USA alone, and among those patients, the deep venous reflux population is close to two million people. Erin Murphy (Charlotte, USA) and Marc Glickman (Irvine, USA) put forward these figures to set the scene for a deep dive into deep venous valvular reflux during a recent CX Vascular Live discussion. They were joined by Ramon Varcoe (Sydney, Australia) to outline the scale of the issue, as well as potential solutions in the pipeline.
“The population is large, it is being treated most of the time with conservative therapy, so I think there is a large demand—untreated, unmet and underdiagnosed,” said Glickman in summary of the overarching issue. “This is a large unmet need worldwide.” Moving beyond the US statistics, he stressed that India, China and Brazil have even larger patient populations with deep venous reflux.
Varcoe concurred that deep venous reflux represents an “enormous global burden,” not only in terms of healthcare costs, but also in patients’ livelihoods. To this point he described the difficulties associated with living with venous ulcers, and the fact that vascular surgeons “really struggle” with these patients in terms of applying compression therapy and using other conservative measures.
Murphy, director of the venous and lymphatic programme at Atrium Health’s Sanger Heart & Vascular Institute, noted that there has been “considerable progress” over the last 10 years in treatment options for patients with reflux in the superficial system, and also in the deep venous obstruction space, with various new stents now available. “Why do you think it is taking so long to establish new technology in the deep venous valve realm?” she posed to the panel.
“For the last 50 to 60 years, everyone has considered finding a cure for deep venous valvular reflux as the holy grail of deep venous disease,” remarked Glickman, highlighting the importance of, and difficulty associated with finding a solution to, the problem. He put forward two issues at play here—one is the challenging nature of correctly diagnosing deep venous valvular insufficiency and the other, a lack of standardisation in making that diagnosis, resulting in the severity of the disease being “missed throughout the medical community”.
Varcoe also stressed the “huge variability” in how this disease is diagnosed, and mentioned another issue, that surgery in these patients is “next to impossible” due to challenging anatomical conditions.
Glickman also noted another challenge in the fact that vascular surgery training tends to focus on arterial disease and less on the venous world, resulting in only “very minor” innovation in the latter.
New technologies “on the horizon”
Glickman expressed his belief that the potential for growth in the deep venous valve market is “enormous”, moving the focus of the conversation towards two new technologies that could improve patient outcomes in this challenging space. On this note, Varcoe expressed his excitement that there are some new technologies “on the horizon” that “might make a huge difference to patients’ lives”.
Glickman is the senior vice president and chief medical officer at Envveno Medical, the company behind the VenoValve, and shared that his training as a vascular surgeon informed him that “most of our endovascular procedures have started out as open procedures that have worked and that have migrated to endovascular,” citing the examples of carotid stenting, ablation and stripping, and the treatment of abdominal aortic aneurysms. In the deep venous reflux space, however, he noted that an open surgical technique is missing.
About seven years ago, Glickman recalled, the VenoValve was developed. He detailed that it is made from a porcine aortic monocusp on a stainless steel frame that is surgically implanted into the femoral vein in the mid-thigh region. The procedure takes about an hour and 15 minutes.
Glickman noted that three-year data from a first-in-human trial conducted in Colombia, which were recently shared at the 2023 American Venous Forum, showed improvement in reflux time, improvement and consistency of the Venous Clinical Severity Score (VCSS), and a reduction in pain. The team are presently conducting another trial—SAVVE—at 24 sites in the USA.
He highlighted that the company is now working on a transcatheter version of its VenoValve device, with the plan being to commence a first-in-human study.
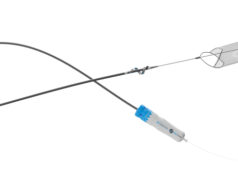
Varcoe, who has been involved in clinical studies on the BlueLeaf (InterVene), shared that this novel device is “completely different” to the VenoValve. “What we do with this device is we make a valve leaflet from the blood vessel wall itself—so we leave nothing behind, we are not transplanting anything, we are literally creating a flap-like valve, which can be either monocuspid or bicuspid and it can be done multiple times in the same vein segment,” he explained. The device is percutaneous, Varcoe added, and is therefore inserted over a guidewire, with the procedure guided by both intravascular ultrasound and fluoroscopy. “It takes around an hour and a half to make a series of valves and we hope that over time those valve cusps endothelialise and become part of the native structure of the vein wall,” he said.
In terms of data, Varcoe noted that 41 patients have now been enrolled in a global clinical trial of the technology. The data demonstrate the safety and efficacy of the device in its early stages, Varcoe reported, and that the procedure can be done without creating deep vein thromboses, which was an “initial fear”. He added that the data have shown some “dramatic, remarkable improvement” in VCSS scores. “Patients I have seen who have had ulcers for 20 years have had them healed within six weeks, and that is extremely satisfying,” he shared.
In addition to VenoValve and BlueLeaf, Cook Medical announced earlier this summer that the first patient has been treated in a clinical study to evaluate a new venous valve designed for treating chronic venous insufficiency (CVI). The patient was treated by principal investigator Mauricio Alviar (Barranquilla, Colombia). The valve’s safety and efficacy are now being tested in a global, multisite clinical trial. The global principal investigator of the study is Paul Gagne (Darien, USA). “When leg veins function poorly, patients suffer with leg swelling, leg pain, leg ulcers, disability, and possible amputation. Therefore, it is important to restore blood flow out of the leg veins, back to the heart. Part of doing this successfully required restoring the function of the venous valves,” Gagne said in a press release at the time.
What is next?
While these technologies are in their infancy, both Glickman and Varcoe are cautiously optimistic about the future. Glickman noted that the focus at Envveno Medical will be finishing up the trial for US Food and Drug Administration (FDA) approval by the end of this year, after which it will take six months to get the approval. The plan is to conduct a large trial in the USA. He summarised that the percutaneous device is probably five years out, and VenoValve “probably two years out from being in people’s hands”.
Jorge Ulloa (Bogota, Colombia), one of the key figures behind research of the surgical VenoValve, told Vascular News the future looks bright in the venous valve space following 65 years of development. “So far, we are at the pivotal phase of the study [of the surgical version of the valve],” he said, relaying how more than 50 cases have now been performed in the USA to date. This follows the first-in-human trial carried out at Ulloa’s institution in Bogota. The surgical valve “seems to have a promising future, due to the length and results from the follow-up, that we have presented extensively in the last three years,” the Fundacion Santa Fe-Universidad de los Andes vascular surgeon continued. “There is another player from Cook Medical, which has already implanted a first device via endovascular deployment, and we are on the way to migrating to [an endovascular device] also.” Ulloa is similarly involved in the first-in-human trial of the endovascularly delivered version of the valve. In the meantime, continuing study of the surgical valve is showing “a plateau in terms of stabilisation in pain, VCSS and reflux time,” he said. “It means that there is no tendency to return to baseline at 36 months of follow-up. That is something that has never happened in previous series, and everything looks like it will continue this way. Of course, only time and follow-up of these cases will show us the path to continue.”
Ulloa believes more new technology will emerge in the venous valve space in the coming years. “I envision a myriad of new devices that will emulate our experience,” he said. “Some will work, some [will not]. So far, there are more than four major companies designing their own concepts, and they will have to run through all the necessary stages in order to prove that they are safe and functional. All of these efforts will only benefit PTS [post-thrombotic syndrome] patients—and that is a good thing.”
On BlueLeaf, Varcoe stated that the team involved is “in a process of innovating and iterating the device”. It is about to launch the fourth generation of the device, which allows for the treatment of larger veins and the creation of more circumferential valve cusps. He added that the company is going through the pre-submission process with the FDA about what an investigational device exemption trial might look like, which it hopes to be able to start within months. “I see a future where this technology is successful,” Varcoe averred, “whichever deep valve technologies do end up being available to us.”
There will undoubtedly be challenges along the way, however. Glickman acknowledged that paradigm shifts in medicine “take time”, emphasising the complexity of the regulatory landscape. He also pointed out the importance of continued education in this space to address a lack of understanding of deep venous insufficiency within the medical community.
“I have just really enjoyed seeing the focus be put back on venous disease,” Varcoe said in closing. “I am seeing huge interest in venous disease now and it is a really great time to be involved in the field.”