
Ramona Gupta (Northwestern University, Chicago, USA) addresses the issue of recurrent varicose veins, highlighting in particular the “multiple tools” now at physicians’ disposal to treat the problem.
Superficial venous insufficiency and varicose veins affect approximately 23% of adults worldwide. Treatments have significantly evolved from surgical ligation and stripping to less invasive endovascular ablative procedures. However, recurrent varicose veins are common with both surgical and endovascular techniques. Durability is an important long-term outcome measure. Recent studies have examined recurrences following endovenous procedures and delineated the rates of recurrence, the patterns of recurrence, and factors associated with recurrence.
Recurrence rates following endovenous ablation procedures has consistently proven lower in long-term studies when compared to ligation and stripping. Multiple studies have confirmed durable closure rates approaching 95% after five years with the thermal and non-thermal ablative technologies. Recurrent rates after ligation and stripping have been described ranging from 20–80% with incidence increasing over time.
Importantly, the recurrence patterns following endovenous ablation are significantly different from those following ligation and stripping. The REVAS (Recurrent varices after surgery) study evaluated a large cohort of patients and found that 20% of recurrences were due to saphenofemoral neovascularisation, 19% of recurrences were secondary to incorrect junctional ligation and 55% of recurrences originated from perforator reflux. Neovascularisation after endovenous ablation is rarely seen. Instead, the majority of recurrences are due to recanalisation of a segment of previously treated vein or new reflux in an accessory saphenous vein or alternate truncal pathway. Specifically, recanalisation of a previously treated great saphenous vein (GSV) or reflux in the anterior accessory great saphenous vein (AAGSV) are common causes of recurrent disease in patients.
Treating these patterns of recurrence often involves employing non-thermal techniques. Recanalised short segment GSV can be effectively treated with ultrasound-guided foam sclerotherapy (USGFS) with special attention to newly refluxing perforator veins frequently noted in the thigh. Recurrent disease with new reflux in the GSV below the knee can be treated with cyanoacrylate adhesive closure or USGFS to avoid nerve injury. The AAGSV frequently becomes superficial, tortuous and outside the sheath after only a few centimetres. Endovenous laser ablation is successful in treating to the saphenofemoral junction although tumescing outside the sheath and achieving adequate depth to prevent a skin burn can be difficult. Cyanoacrylate adhesive closure requires 10cm of straight segment to treat. USGFS is an option but has routinely demonstrated lower closure rates. The short saphenous vein is also a common culprit for disease recurrence and can be successfully treated with most of the newer technologies, thermal or non-thermal.
Factors related to varicose vein recurrence after endovenous ablation include: 1) obesity with increased abdominal pressure increasing the likelihood of venous reflux, 2) increase in the diameter of the vein to be treated and 3) treated refluxing venous segment below the knee.
While awareness of these factors is important, they rarely cause me to alter my treatment or post-treatment plan. However, I do council patients that recurrence may be more likely in these situations and I encourage vigilant use of compression in the immediate- and long-term post-treatment period.
In my practice, recognising and treating recurrent disease is an important factor in overall long-term leg health and patient satisfaction. Our practice does not routinely bring patients back at one year for follow-up ultrasound so most recurrences are noted solely due to return of symptoms or new visible varicosities. In addition, recurrences can be a significant cause of morbidity as seen in the case below.
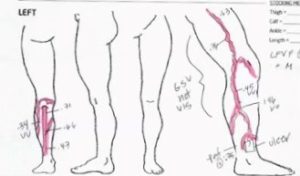
Figure 1 is the map of a patient who was treated with endovenous radiofrequency ablation of the GSV at an outside clinic five years prior to her presentation in my clinic. Her standing duplex ultrasound examination demonstrates several important patterns of recurrence: perforator reflux and new small saphenous vein (SSV) reflux. Moreover, she had a large non-healing wound at the medial malleolus, which had been present for six months (Figure 2).

I treated her in a single session with endovenous laser ablation of the SSV and USGFS of the refluxing varicosities in the thigh and calf. She followed a strict regimen of compression and wound care following the procedure. At six months, the wound showed significant healing and the patient reported meaningful improvement in her swelling and heaviness (Figure 3).

While recurrent varicose veins can be frustrating for the patient and the physician, rates of recurrence are low with newer techniques and patterns of recurrence are easily recognisable. Physicians have multiple tools available to treat these new refluxing veins and are able to achieve excellent clinical outcomes.
Ramona Gupta is associate professor of radiology at Northwestern University in Chicago, USA.












