In a comparison of endovascular versus hybrid treatment of chronic venous obstructions (CVOs) involving the confluence of the common femoral vein, researchers have found that both strategies provide similar patency rates. Writing online in the Journal of Vascular Surgery: Venous and Lymphatic Disorders, Long Piao (University Hospital Aachen, Aachen, Germany) and colleagues specify that an endovascular strategy has the benefit of fewer postoperative complications and a shorter procedure duration and hospital stay compared with the hybrid approach.
The authors state that treatment of extensive CVO with post-thrombotic trabeculation involving the common femoral vein or deep femoral vein remains a challenge, with a lack of clarity on the best treatment technique for such cases. In the present study, therefore, the investigators compared the results of endovascular alone versus endovascular with additional endophlebectomy, or hybrid, procedures for such patients.
The research team retrospectively reviewed the medical records of 102 consecutive patients (108 limbs) treated between 2015 and 2020 for iliofemoral CVO extending to the femoral confluence. They detail that the patients were divided into two groups: the hybrid procedure and endovascular treatment groups.
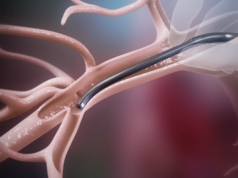
The hybrid procedure group consisted of those treated with stent implantation and endophlebectomy of the common femoral vein with the creation of an arteriovenous fistula, whereas the endovascular treatment group included those who had undergone stent implantation alone, Piao et al relay.
Of the 102 patients included in the study, the authors specify that 47 (49 limbs) were in the endovascular group and 55 (59 limbs) were in the hybrid procedure group. They note that the demographics of the two groups were similar with no statistically significant differences in cumulative primary (33.7% vs. 36.3%, p=0.839), assisted primary (59.8% vs. 64%, p=0.941) or secondary patency rates (69% vs. 72%, p=0.851) at 36 months. They add, however, that the patients in the endovascular treatment group had better clinical improvement with a lower postoperative complication rate (p=0.012), shorter procedure duration (p<0.001) and shorter hospital stay (p=0.025).
Piao and colleagues acknowledge certain limitations of the present study, urging that the results should be interpreted with caution because they are based on a retrospective analysis of a small cohort of patients. Among other drawbacks, they recognise that the decision to perform endophlebectomy according to the intraoperative imaging findings could have led to bias in patient allocation.