
At the American Venous Forum meeting (14–17 February, New Orleans, USA), Johann Christof Ragg (Berlin/Zurich, Germany/Switzerland), presented on the concept of obtaining ultrasound proof of pre-reflux stages of venous insufficiency. Ragg spoke to Venous News about what light his data can shed on the origins of the condition and how this research could impact clinical practice.
What explanations have previously been given to the origin of venous insufficiency?
The cause of venous insufficiency has been said to be mainly genetic. There are more than 20 genetic code locations for relevant properties of veins, and sometimes certain families seem to be struck with that disease. However, we showed in a recent pilot study that up to 25% of young people (8–16 years in age) have valve lesions. These include missing valves or valve parts and lesions of valves, with local reflux and dilatation or reflux of superficial veins in 50% of cases. In other words, we found early stages of insufficiency due to congenital valve defects. Later on, these are blurred by acquired insufficiency of different patterns, which we presented at the American Venous Forum.
There are three factors of degenerative changes in leg veins. First, shear stress due to blood flow (“normal”); second, wall stress, dilatation and thickening due to congestion; third, inflammatory and prethrombotic changes predominantly in valve regions due to stasis. Long-term addition and combination of these stress types lead to what we see in adults, with or without evident disease. Genetics are just a co-factor, contributing to a more or less accelerated course of the disease.
Can you tell us about the ultrasound systems used in this study?
Using high frequency broadband ultrasound, offering up to 70MHz while still obtaining imaging in 3–5cm depth by application of sophisticated filter algorithms, signals are obtained from moving, clotting or wall-adhering blood particles superior to known B-flow imaging. For that study, we used the novel Vevo MD (30MHz) (Fujifilm SonoSite), as well as the Acuson X700 (16MHz) (Siemens Healthineers).
What is the relevance of microaggregates in this context?
Microaggregate formation of blood cells occurs in leg veins in a fully reversible way during slow or stagnant flow; the phenomenon is called “sludge”. In contrast, we frequently see aggregates in the valve sinus or adhering to valve structures which do not resolve or disappear, no matter how hard the patient tries to generate vein flow, or we try to do so through methods such as calf compression. We called these “permanent” or “persistent” aggregates and registered them by collecting video sequences pre- and post-intense motion. Furthermore, we analysed the cusps for the presence of increased signal intensity, increased wall thickness or roughness of surface.
What results were reported from your study?
We compared vein valves in three groups of patients, with 40 in each group, all with inconspicuous findings in routine vein sonography:
- Group A: >10 years in professions with >6 hours of daily sitting, showing permanent aggregates in 47.5% of cases;
- Group B: >10 years in professions with >6 hours of daily standing, showing permanent aggregates in 45% of cases;
- Group C: Patients with a similar long history in “healthy” professions with <2 hours of daily sitting or standing, including postmen, bicycle couriers, forest inspectors or sport professionals, showing permanent aggregates in 25% of cases.
The frequency of all valvular pathologies was approximately twice as high in all three groups (90%, 92.5%, and 47.7%, respectively). The clinical conclusion was that permanent aggregates were much more frequent in cases with long and daily phases of stasis or congestion. However, valve degeneration may also occur in subjects with “healthy” professions; maybe they returned home from work and spent the rest of the day lying on the couch. In further studies, we will try to collect data on 24-hour motion habits. Nevertheless, the preliminary findings on permanent aggregates strongly suggest a relation to the well-known inflammatory changes in vein valves during the course of venous insufficiency. Maybe we found the missing link; a proof of stasis leading to inflammation via aggregate adhesion and interaction.
Were there any notable results in the study’s subgroup(s)?
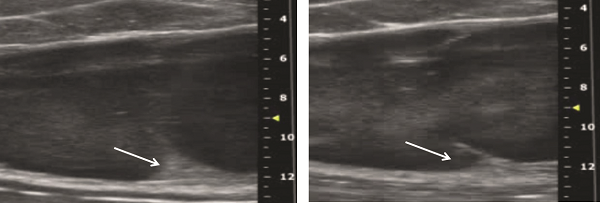
A subgroup of 12 cases with 26 aggregate-related valves from standing or sitting professions started to wear medical compression stockings (23–32 mmHg) and do 30 minutes of daily walking. After three months, reduction of aggregates was detectable in 21/26 (80.8%) related valves (Figure 1).
From your observations, what conclusions can be drawn?
Obviously, we found some visual parameters for the detection of progressive venous disease, in particular for early and pre-reflux stages, which might offer great chances for conservative treatment. Criteria for quantification and correlation to histology will now have to be established.
How do you hope this will influence future research or current practice?
The criterion of permanent blood particle aggregates may serve as a new parameter in the evaluation of conservative vein treatment. For the first time, treatment effects on valve shape and function become directly and non-invasively accessible, with tremendous impact on future indications for compression stockings, physical exercise or medication.









