An updated guideline on the prophylaxis and treatment of venous thromboembolism (VTE) in patients with cancer has been unveiled by the American Society of Clinical Oncology (ASCO) in its Journal of Clinical Oncology. An expert panel convened by ASCO reviewed evidence—including randomised controlled trials (RCTs) and meta-analyses of RCTs—from the period between 1 August 2014 and 4 December 2018, before providing a list of findings and recommendations.
Patients with cancer are at a higher risk of developing VTE, including deep vein thrombosis (DVT) and pulmonary embolism (PE), than those without cancer, and have higher rates of VTE recurrence and bleeding during VTE treatment. Consequently, VTE is an “important cause of morbidity and mortality” among cancer patients.
According to the review, two RCTs of direct oral anticoagulants (DOACs) for the treatment of VTE in cancer patients confirmed the efficacy of edoxaban and rivaroxaban, but found that they could be associated with an increased risk of bleeding compared to low-molecular-weight heparin (LMWH). Furthermore, two additional RCTs underlined the potential benefits and side-effects of DOACs for thromboprophylaxis in ambulatory cancer patients at a higher risk of VTE.
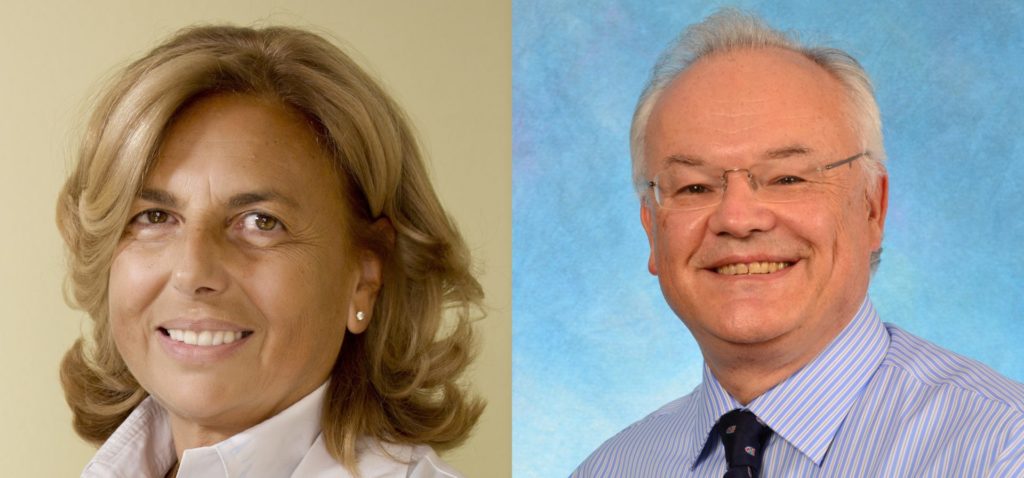
Co-chaired by Nigel S Key (Chapel Hill, North Carolina, USA) and Anna Falanga (Bergamo, Italy), the panel’s systematic review included a total of 35 publications (26 meta-analyses and nine RCTs) on VTE prophylaxis and treatment, and 18 publications on VTE risk assessment (six included multiple types of cancer, while 12 focused on individual cancer types). In addition to Key and Falanga, 15 additional authors worked on the project.
Speaking to Interventional News about the importance of these guidelines, Key comments, “This iteration of the ASCO guidelines on VTE prevention and treatment reflects an evolving evidence-based set of recommendations on a common problem in a challenging patient population. Perhaps the greatest advances are the recommendations to consider certain oral direct factor Xa inhibitors for the treatment of VTE and for VTE prevention in higher risk cancer patients.”
Falanga is in accordance, adding, “The updated ASCO guidelines reflect the new evidence from clinical research showing the efficacy of new anticoagulant drugs for VTE management in oncology. The addition of some DOAC to our armamentarium to prevent and treat cancer-associated VTE expands our choice and allows the possibility to personalise treatment based on patient characteristics and type of cancer.”
The updated guideline addresses six clinical questions:
- Should hospitalized patients with cancer receive anticoagulation for VTE prophylaxis?
- Should ambulatory patients with cancer receive anticoagulation for VTE prophylaxis during systemic chemotherapy?
- Should patients with cancer undergoing surgery receive perioperative VTE prophylaxis?
- What is the best method for treatment of patients with cancer with established VTE to prevent recurrence?
- Should patients with cancer receive anticoagulants in the absence of established VTE to improve survival?
- What is known about risk prediction and awareness of VTE among patients with cancer?
In response to the first clinical question, “Should hospitalized patients with cancer receive anticoagulation for VTE prophylaxis?”, ASCO’s guideline states that hospitalised patients who have active malignancy and acute medical illness, or reduced mobility, should be offered pharmacologic thromboprophylaxis in the absence of bleeding, while patients with active malignancy but no additional risk factors may be offered pharmacologic thromboprophylaxis. However, pharmacologic thromboprophylaxis should not be offered to patients admitted for minor procedures or chemotherapy infusion, nor patients undergoing stem-cell or bone marrow transplantation.
On the subject of whether ambulatory patients with cancer should receive anticoagulation for VTE prophylaxis during systemic chemotherapy, a new addition to the guideline is that high-risk outpatients with cancer may be offered thromboprophylaxis with apixaban, rivaroxaban or LMWH Patients with multiple myeloma receiving thalidomide or lenalidomide with chemotherapy should be offered pharmacologic thromboprophylaxis, according to the guideline.
For cancer patients undergoing surgery, it is recommended that all persons with malignant disease undergoing a major surgical intervention receive perioperative VTE prophylaxis with either unfractionated heparin (UFH) or LMWH, unless they present a high bleeding risk or other contraindications. Prophylaxis should be commenced preoperatively and continue after surgery for at least seven to 10 days, while extended prophylaxis with LMWH, for up to four weeks, is recommended for cancer patients undergoing major open, laparoscopic abdominal or pelvic surgery.
Regarding the best method of treating cancer patients in order to prevent VTE recurrence, a number of recommendations are included in the guideline. Initial anticoagulation may involve LMWH, UFH, fondaparinux, or rivaroxaban, though LMWH is preferred over UFH for the initial five to 10 days of anticoagulation for patients with newly diagnosed VTE. For long-term anticoagulation of six months, it is stated that LMWH, edoxaban, or rivaroxaban are more effective and therefore preferred. Patients with active cancer, including those with metastatic disease or persons receiving chemotherapy, should receive anticoagulation with LMWH, DOACs or vitamin K antagonists (VKAs) beyond six months.
Responding to expert opinion in the absence of randomised trial data, uncertainty towards short-term benefits, and evidence of long-term harm from filters, ASCO has recommended against the insertion of a vena cava filter for patients with established or chronic thrombosis. Additionally, the guideline asserts that filter insertion has no role for primary prevention or prophylaxis of PE or DVT, though a vena cava filter may be offered as an adjunct to anticoagulation in patients with progression of thrombosis. Incidental PE and deep vein thrombosis should be treated in the same manner as symptomatic VTE, according to ASCO.
Answering the question of whether patients with cancer should receive anticoagulants in the absence of established VTE to improve chances of survival, anticoagulant use is not recommended to improve survival in patients with cancer without VTE.
Finally, the guideline addresses what is known about risk prediction and awareness of VTE among patients with cancer, recommending that those persons should be assessed for VTE risk initially and periodically, particularly when starting systemic antineoplastic therapy or at the time of hospitalisation. At the same time, individual risk factors do not reliably identify patients with cancer at high risk of VTE. ASCO argues that oncologists should educate patients regarding VTE, particularly in settings that increase risk such as major surgery and hospitalisation.









