Data from the LAMA (Laser ablation versus mechanochemical ablation) trial indicate that mechanochemical ablation (MOCA) is significantly less painful than endovenous laser ablation (EVLA) during treatment of superficial venous incompetence, though there is no difference in pain between the two treatments when the pain of phlebectomy is taken into account. Both techniques significantly improved clinical severity and quality of life in this trial.

Presenting the results at the European Society of Vascular Surgery (ESVS) annual meeting (19–22 September, Lyon, France), Clement Leung (University of Hull, UK)—on behalf of fellow investigators and supervisor Ian Chetter (Hull and East Yorkshire Hospitals NHS Trust, UK)—told the audience that post-procedural pain was also less in the MOCA group, though this had no apparent clinically-significant effect.
“EVLA is the recommended first-line treatment for superficial venous incompetence,” Leung told ESVS delegates. “However such thermal technique requires tumescent anaesthesia, which can be uncomfortable for the patient. Newer non-thermal techniques such as MOCA aim to remove or reduce the need for tumescent and thus reduce pain.”
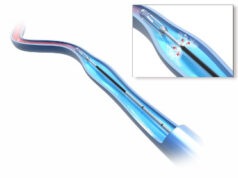
The single-centre, randomised, controlled LAMA trial compared the two treatments with follow-up at one week, six weeks and six months. The trial enrolled 82 patients, of which 72 attended six-month follow-up. Patients underwent either MOCA (ClariVein, Vascular Insights; n=41) with 1.5% sodium tetradecyl sulphate or EVLA (n=41) with 1,470m, NeverTouch gold-tip fibre (AngioDynamics). Concomitant phlebectomy was performed on symptomatic visible varicosities. The mean age of all randomised patients was 53 years and 59% were female. Both groups were well-matched at baseline.
The trial’s primary outcome measure was intra-procedural pain scores on a 100mm visual analogue scale (VAS). Secondary outcomes included post-procedural pain scores, clinical severity scores, general and disease-specific quality of life measurements, recovery time, and duplex ultrasound assessment.
Leung reported that patients in the MOCA group experienced significantly less pain during truncal ablation with MOCA (median 10mm, range 9–24mm) compared with EVLA (median 28mm, range 19–59mm, p=0.01). However, he noted that this benefit was lost following concomitant phlebectomy, and that there was no significant difference in the overall pain scores by the end of the procedure (MOCA median 29mm vs. EVLA median 38mm, p=0.441).
Patients in the MOCA group also experienced less pain during the next six post-procedural days (by 5mm vs. 14mm, p<0.05). There was no significant difference between the groups for either return to work (MOCA median seven days [range 4–14 days] vs. EVLA median six days [range 4–14 days], p=0.812) or return to normal activities (MOCA median two days [range 1–3 days] vs. EVLA median three days [range 1–7 days], p=0.169). Technical success (MOCA 92% vs. EVLA 94%), clinical severity scores and disease-specific quality of life scores were similar between groups at six weeks and six months. There were no significant complications.
“During truncal ablation, MOCA is less painful than EVLA, but this benefit is lost if concomitant phlebectomy is performed,” Leung concluded. “MOCA appears less painful during the first post-procedural week, while both have similar recovery time, clinical improvement, short-term technical success, quality of life improvement and safety outcomes. Longer follow-up is now required.”