This article is sponsored by the European College of Phlebology.
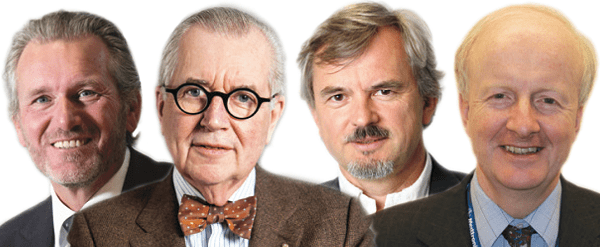
It is a fact that the incidence of venous disease is rising; currently, 25% of Europe’s population is affected, and this figure will climb to 35% by 2050. Due to an ageing population and increased levels of obesity, a clear plan and future perspective is needed, not only to battle the burden of this disease on patients, but also because it accounts for at least 1% of national healthcare budgets throughout Europe. In this article, Cees Wittens, Martino AM Neumann, Eberhard Rabe and Alun H Davies explain how the European College of Phlebology is working towards this goal.
During the last decade, there have been many changes in the management of patients suffering with venous disease. The treatment of superficial venous insufficiency, for instance, has shifted from invasive treatments under general anaesthesia to minimally invasive treatments under tumescent anaesthesia. Equally, the treatment of incompetent perforating veins became more popular due to the introduction of endoscopic surgery, which has already been completely replaced by percutaneous techniques.
Similarly, the management of chronic venous disease, due to deep venous insufficiency (DVI) and deep venous occlusive (DVO) disease has undergone major changes. In the past, more attention was paid to treat DVI, but in the last decade the burden of a deep venous outflow obstruction, mostly as a complication of a deep venous thrombosis (DVT), has been re-evaluated and is now considered of much more relevance than DVI. It has also been shown that DVO disease is treatable with new, minimally invasive techniques such as recanalisation, which involves stenting of the pathological venous segments, especially in the iliofemoral tract.
A more aggressive treatment has been introduced to treat DVT as well, with the expectation that removing the clot in acute DVT (especially an iliofemoral DVT) will significantly reduce the burden of a post-thrombotic syndrome. Recent studies challenge this statement, but it has been shown that just half of the patients receiving an intervention were treated successfully in those studies. However, when the clot was successfully removed, the post-thrombotic syndrome burden significantly reduced, indicating the need for better techniques and tools.
Compression bandaging and stockings still remain the cornerstone for the treatment of numerous patients with venous disease; most compression innovations focus on short-stretch bandaging because of its higher efficacy and comfort. Finally, the introduction of new anticoagulant drugs is changing the treatment options available for venous disease, improving the comfort and safety of patients. These developments, as highlighted above, require the cooperation of industry, physicians and patients. Fast-changing treatment options, due to new inventions, materials and techniques, also place a lot of demand on funders of healthcare—including health insurance providers and governments— to decide which treatments are cost-effective and eligible for reimbursement.
On the other hand, physicians involved in the treatment of patients with venous disease will use the methods they are allowed to use or what fits their expertise, sometimes ignoring potentially better treatment options. Any physician— general, dermatologist, radiologist, surgeon, vascular surgeon, angiologist, cardiologist—can treat patients with a venous disease.
Across European countries, there is great heterogeneity, not only with respect to physician training and speciality, but also in terms of the methods offered to the patient. This is often related to the reimbursement system, which differs in many European countries. To make the situation even more complicated, each country has its own guidelines, often influenced by the specialities involved.
However, patients suffering with a venous disease throughout Europe are very similar. It is the increased awareness of this that should guide us to better-organised care for these patients. Ideally, all of those persons affected by venous disease should receive the best reimbursed medical care in each country, according to the highest standards.
In fact, one guideline throughout Europe should be sufficient, and all physicians involved should be trained and taught to the level needed to provide optimal care.
In order to realise a higher standard of care across the continent, the International Union of Phlebology (UIP) has already developed a curriculum for phlebology. While the educational programme, published in 2010, covers all aspects of care for these patients, it is difficult to use as a multidisciplinary tool.
The European College of Phlebology (ECoP) was established in 2012 with the mission of achieving optimal care for all patients in Europe suffering from a venous disease. The patient has the expectation to be treated by a well-trained physician. In order to know if a physician is educated and appropriately trained to perform appropriate diagnostics and treatment, a Certificate of Phlebology needed to be established. Such a certificate would show the patient, and patient organisations, that an appropriate physician will treat the patient.
With the help of standardised education and training, quality of care should improve throughout Europe. To get an internationally accepted Certificate in Phlebology and allow free movement throughout Europe for a Certified Phlebologists, recognition by the European Union of Medical Specialists (UEMS) is essential.
After the ECoP supported the foundation of a Multidisciplinary Joint Committee of Phlebology (MJCP) in 2014, the European Board of Phlebology (EBP) was installed by the MJCP in 2017 (within the UEMS), and is responsible for the education, training and certification of phlebology in Europe. The EBP succeeded in acceptance of official training requirements for National Reference Training Centres in Phlebology (NRTCP), European Training Centres of Phlebology (ETCP), European Rotation Training Centres in Phlebology (ERTCP) and Trainers, improving the level of care significantly.
According to UEMS, its aims are: “To promote and harmonise the highest level of training of medical specialists, medical practice and healthcare within the EU; to promote free movement of specialists within the EU; to legally represent the medical specialist in the Member States of the EU dealing with questions directly or indirectly concerning the medical profession; to defend the professional interests of European Medical Specialists.”
The EBP educational programme focuses on the practical training of skills needed to diagnose and treat patients with venous diseases. This will be covered by the selected European Training Centres.
Alternatively, the ECoP will be focusing on the theoretical part of the educational programme and is offering a the ECoP e-Learning Course. Th ECoP e- Learning Course 2021 is finished in November 2021 with 75 participants from all over the world. The ECoP is also running a physical Course from 26–28 November, 2021 in Amsterdam, the Netherlands, and provide the participants an overview of the main venous topics. In 32 workshops the course will demonstrate the discussed diagnostic and treatment options in practice.
The ECoP represents most of the 24 national phlebology societies in Europe and will support them in developing guidelines, education and training programmes.
In order to further support this vision, the ECoP is intending to foster European guidelines, covering best medical care for the venous patient in Europe, provided by a certified physician. These guidelines will show conclusions, based on sound principles of best available evidence. Moreover, the recommendations will be made in cooperation with each individual phlebological society, because of the local legal and social situations.
In the near future, appropriate certified physicians should treat patients with venous disease according to international multidisciplinary guidelines, and all health workers, patients and related industries involved in the care for these patients should collaborate to guide the quality of care.
Finally, the aim of ECoP is to engender cooperation between all European societies and institutions involved in the diagnosis and treatment of acute and chronic venous diseases, as well as maintaining multidisciplinary phlebology across Europe.
Cees HA Wittens is a vascular surgeon who has dedicated the last two decades of his practice and research to venous pathology.
Martino AM Neumann is a dermatologist and, between 2002 and 2015, was head of the department for dermatology and venereology at the Erasmus MC, Universitair Medisch Centrum Rotterdam, the Netherlands.
Eberhard Rabe became a professor of dermatology in 2002, and is is currently president of the European College of Phlebology.
Alun H Davies is a professor of vascular surgery and head of section of vascular surgery at Imperial College London. The authors have no disclosures.












